
Dr. Fawaz Al Ammary received his medical degree from Cairo University School of Medicine. He completed his Internal Medicine residency training at Case Western Reserve University (MetroHealth) in Cleveland, Ohio, and nephrology and transplant nephrology fellowship training at the University of Colorado in Denver, Colorado. He also completed a Ph.D. in health services research at the University of Colorado.
Dr. Al Ammary served as a full-time faculty member and medical director of the living kidney donor program in the Division of Nephrology, Department of Medicine at Johns Hopkins University from 2015 to 2022, and then he joined the University of California, Irvine in December 2022 as an Associate Professor and a senate faculty member.
Dr. Al Ammary has received National Institute of Health (NIH) Awards, including NIDDK K23 Career Development Award (2021-2026) and NIDDK R03 Award (2025-2027), a National Kidney Foundation, and philanthropic grants. His work broadly focuses on advancing access to living donor kidney transplantation and leveraging telemedicine services to improve transplant care accessibility for diverse populations. Parallel to this, Dr. Al Ammary serves as Chair of the Telemedicine Workgroup, American Society of Transplantation Living Donor Community of Practice (2020-current).
ORCID https://orcid.org/0000-0003-0928-2860
LinkedIn https://www.linkedin.com/in/fawazalaammary/
Racial and ethnic disparities in preemptive kidney transplantation in the United States
Fawaz Al Ammary1, Abimereki D. Muzaale1, Simeon Adeyemo1.
1Medicine, University of California, Irvine, Irvine, CA, United States
Living Donor Transplant Outcome Collaborative (LDTOC).
Background: Preemptive (prior to dialysis initiation) kidney transplantation improves survival and reduces costs. While prior research documented racial/ethnic disparities in preemptive referrals, less is known about distinct outcomes following preemptive waitlisting. We examined the association between race/ethnicity and outcomes over time among adult CKD patients who were preemptively waitlisted for kidney transplantation in the United States.
Methods: We analyzed data from the Scientific Registry of Transplant Recipients (SRTR), including 98,936 adult first-time kidney transplantation candidates preemptively waitlisted between January 1, 2009, and December 31, 2020. Primary outcome was living donor kidney transplantation (LDKT), deceased donor kidney transplantation (DDKT), or dialysis initiation within three years of preemptive waitlisting. We used competing risk models to estimate the adjusted subdistribution hazard ratios (aSHRs) of an event with competing risks including death, accounting for demographic, health, and socioeconomic factors. Data were stratified into three-year increments (2009–2011, 2012–2014, 2015–2017, and 2018–2020).
Results: Among 98,936 preemptively waitlisted adults (median [IQR] age, 56 [46–64] years; 42% women), 60% were White, 19% Black, 13% Hispanic, 8% Asian. In every era, Black, Hispanic, and Asian patients were less likely to receive preemptive LDKT than White patients (era 2018–2020, aSHRs: 0.31 [95%CI, 0.29–0.34]; 0.60 [95%CI, 0.56–0.65]; and 0.49 [95%CI, 0.44–0.54], respectively). Black, Hispanic, and Asian patients were more likely to initiate dialysis than White patients (era 2018-2020, aSHRs: 1.41 [95%CI, 1.33–1.49]; 1.20 [95%CI, 1.13–1.28]; and 1.50 [95%CI, 1.39–1.61], respectively). In contrast, Black and Hispanic patients received preemptive DDKT as often as White patients (era 2018-2020, aSHRs: 0.99 [95%CI, 0.91–1.07] and 1.01 [95%CI, 0.92–1.11], respectively), while Asian patients were less likely to receive preemptive DDKT (aSHR: 0.77 [95%CI, 0.68–0.87]).
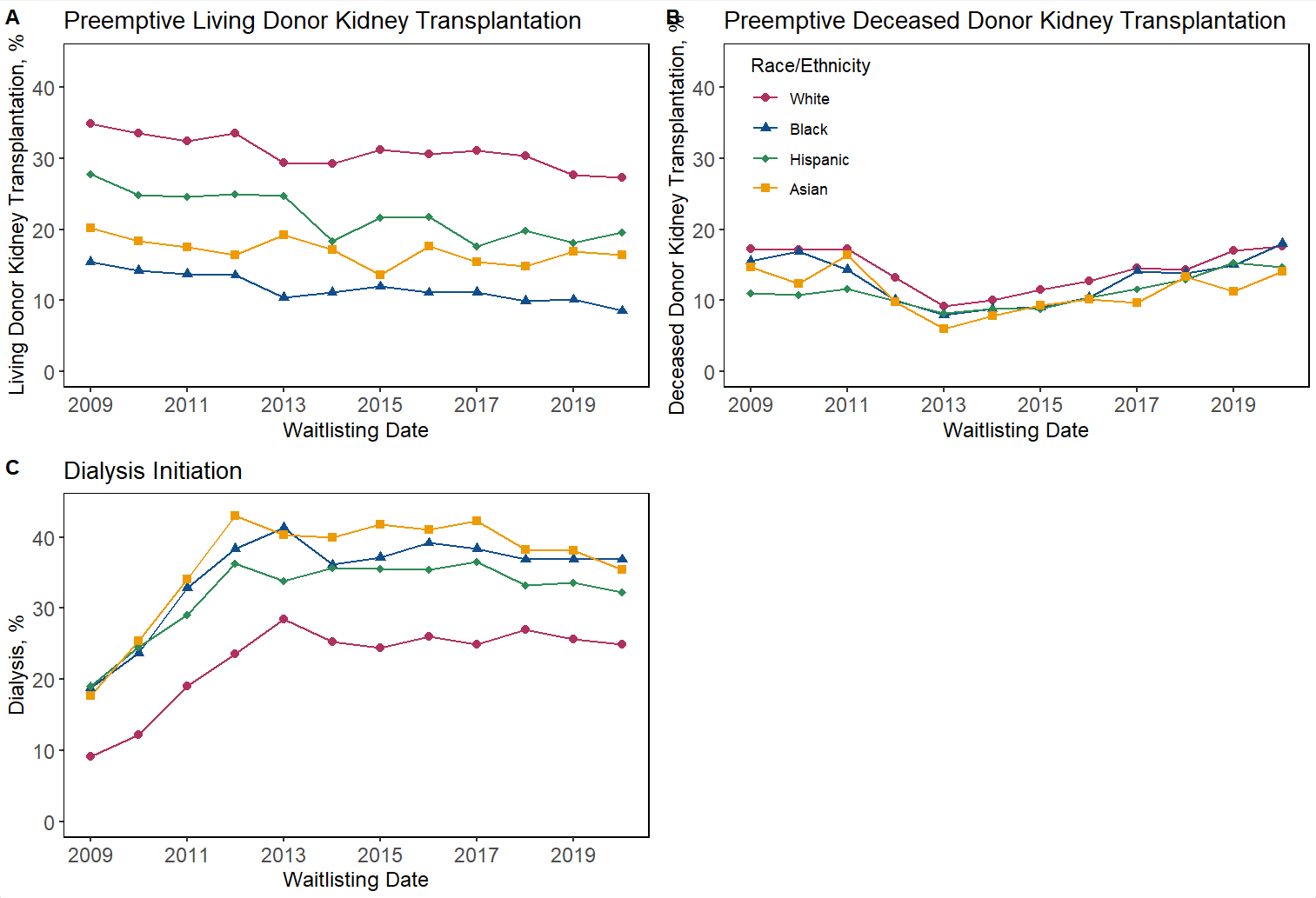
Conclusion: The study highlights persistent disparities in dialysis initiation and LDKT among preemptively waitlisted Black, Hispanic, and Asian patients. Conversely, Black and Hispanic patients had similar rates of preemptive DDKT as White patients. Changes in healthcare practice and policies are needed to expand access to preemptive DDKT and LDKT and maintain equitable, high-quality care throughout the transplant waiting process.
[1] Preemptive kidney transplantation
[2] Living Donor Kidney Transplant
[3] Deceased Donor Kidney Transplant
[4] Preemptive kidney transplant Waitlisting
[5] Outcomes