
Dr. Fawaz Al Ammary received his medical degree from Cairo University School of Medicine. He completed his Internal Medicine residency training at Case Western Reserve University (MetroHealth) in Cleveland, Ohio, and nephrology and transplant nephrology fellowship training at the University of Colorado in Denver, Colorado. He also completed a Ph.D. in health services research at the University of Colorado.
Dr. Al Ammary served as a full-time faculty member and medical director of the living kidney donor program in the Division of Nephrology, Department of Medicine at Johns Hopkins University from 2015 to 2022, and then he joined the University of California, Irvine in December 2022 as an Associate Professor and a senate faculty member.
Dr. Al Ammary has received National Institute of Health (NIH) Awards, including NIDDK K23 Career Development Award (2021-2026) and NIDDK R03 Award (2025-2027), a National Kidney Foundation, and philanthropic grants. His work broadly focuses on advancing access to living donor kidney transplantation and leveraging telemedicine services to improve transplant care accessibility for diverse populations. Parallel to this, Dr. Al Ammary serves as Chair of the Telemedicine Workgroup, American Society of Transplantation Living Donor Community of Practice (2020-current).
ORCID https://orcid.org/0000-0003-0928-2860
LinkedIn https://www.linkedin.com/in/fawazalaammary/
Living kidney donation and obesity: A systematic review and meta-analysis
Fawaz Al Ammary1, Asad Naveed1, Simeon Adeyemo1, Abimereki D. Muzaale1.
1Medicine, University of California, Irvine, Irvine, CA, United States
Living Donor Transplant Outcome Collaborative (LDTOC).
Background: Obesity is a global public health concern. Given the shortage of living kidney donations, transplant centers have been more willing to accept obese donor candidates in recent years. To better counsel obese donor candidates about the risks of donor nephrectomy, we aimed to summarize the evidence on long-term risks for obese living kidney donors compared to non-obese living kidney donors across studies.
Methods: A systematic search of standard databases was conducted to identify studies comparing obese and non-obese living kidney donors. Outcome data were extracted and synthesized. Obesity was defined as a BMI ≥ 30. The risk of bias was assessed using Cochrane's risk of bias in non-randomized studies of interventions (ROBINS-I) tool.
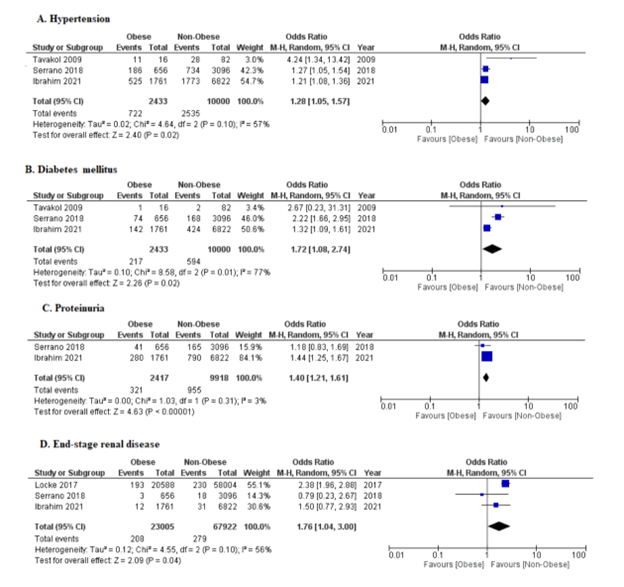
Results: Thirty-three cohort studies were considered in the final review among which only six reported long-term outcomes (Figure 1). Three (3) studies accounting for 12,433 patients showed that obese patients have a significantly higher odds of developing hypertension compared to non-obese patients (OR: 1.28, 95% CI: 1.05-1.57). Similarly, Obese donors have significantly higher odds of developing diabetes mellitus 1.72 (95% CI: 1.08-2.74) and proteinuria (OR = 1.40, 95% CI: 1.21–1.61). Lastly, three studies accounting for 90,927 patients showed that obese donors had a higher odd of developing end-stage renal disease 1.76 (95% CI: 1.04-3.00, p=0.04, I² = 56%). The difference in incidence of cardiovascular disease, creatinine and eGFR in obese versus non-obese LKDs was not significant. The certainty of evidence evaluated using GRADE showed low certainty in three outcomes, moderate in two outcomes and high in two outcomes highlighting confidence in the overall results.
Conclusion: Living kidney donors with obesity have increased risks of developing long-term complications. These findings highlight the need for interventions to minimize perioperative risk for obese donors and tailored follow-up care to ensure the best outcomes for this group of donors, who provide a vital source for living kidney donation.
[1] Living Donation
[2] Obesity
[3] Outcomes
[4] Kidney donation