
Dr. Fawaz Al Ammary received his medical degree from Cairo University School of Medicine. He completed his Internal Medicine residency training at Case Western Reserve University (MetroHealth) in Cleveland, Ohio, and nephrology and transplant nephrology fellowship training at the University of Colorado in Denver, Colorado. He also completed a Ph.D. in health services research at the University of Colorado.
Dr. Al Ammary served as a full-time faculty member and medical director of the living kidney donor program in the Division of Nephrology, Department of Medicine at Johns Hopkins University from 2015 to 2022, and then he joined the University of California, Irvine in December 2022 as an Associate Professor and a senate faculty member.
Dr. Al Ammary has received National Institute of Health (NIH) Awards, including NIDDK K23 Career Development Award (2021-2026) and NIDDK R03 Award (2025-2027), a National Kidney Foundation, and philanthropic grants. His work broadly focuses on advancing access to living donor kidney transplantation and leveraging telemedicine services to improve transplant care accessibility for diverse populations. Parallel to this, Dr. Al Ammary serves as Chair of the Telemedicine Workgroup, American Society of Transplantation Living Donor Community of Practice (2020-current).
ORCID https://orcid.org/0000-0003-0928-2860
LinkedIn https://www.linkedin.com/in/fawazalaammary/
Integrating telemedicine into a hybrid care model in living kidney donor evaluation: A mixed-methods study
Fawaz Al Ammary1, Ivette Nunez1, Simeon Adeyemo1, Christina I. Mejia2, Hannah Sung1,2.
1Medicine, University of California, Irvine, Irvine, CA, United States; 2Department of Medicine, Johns Hopkins Univeristy, Baltimore, MD, United States
Living Donor Transplant Outcome Collaborative (LDTOC).
Background: The evaluation of living kidney donors is a complex, multistage process that involves lengthy in-person visits. Telemedicine offers a promising approach to facilitate the early stages of this process. This study aimed to synthesize expert-informed recommendations to guide transplant centers in integrating telemedicine into a hybrid evaluation model that enhances access to donor evaluation.
Methods: We conducted a two-phase sequential mixed-methods study with multidisciplinary transplant providers in the United States from March 2023 to May 2025. In Phase 1, we held four qualitative focus groups involving 3 surgeons, 5 nephrologists, 7 nurse coordinators, and 9 social workers to explore perspectives on telemedicine in living donor evaluation and identify key themes. In Phase 2, we used a modified Delphi panel method to further examine these themes and develop consensus-based recommendations.
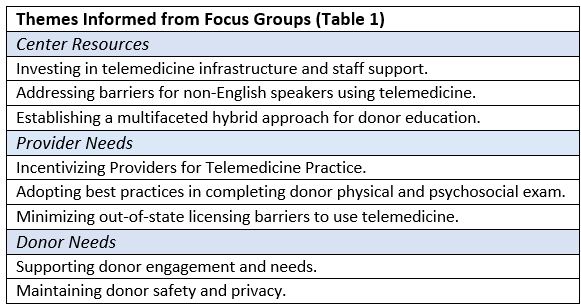
Results: Eight key themes emerged from the focus groups, including center resources, provider, and donor needs.
Based on the themes from focus groups, we proposed 21 preliminary recommendations. In the first round of the Delphi panel, 13 recommendations reached consensus on appropriateness, feasibility, and priority, and advanced to Round 2. In the second round, participants re-ranked the recommendations by priority and rated the extent to which the absence of each would pose a barrier to implementing telemedicine in donor evaluation. Ultimately, 13 recommendations were prioritized by multidisciplinary stakeholders. The top five, listed from highest to moderate priority, were: (1) securing leadership support to strengthen telemedicine infrastructure and enable expansion (mean 4.3, SD 0.66); (2) addressing potential coercion, such as recipient presence during evaluation, by providing alternative private settings (mean 4.2, SD 0.77); (3) offering telemedicine as an option to reduce travel, cost, and disruptions to work or caregiving (mean 3.9, SD 0.64); (4) supporting provider licensure across state lines to accommodate out-of-state donors (mean 3.85, SD 0.81); and (5) establishing a simple telemedicine workflow with real-time staff support (mean 3.75, SD 0.55).
Conclusion: Findings from this rigorous mixed-methods study offer practical guidance for integrating telemedicine into a hybrid model for living donor evaluation. The results underscore the importance of robust institutional infrastructure, provider support, donor-centered flexibility, and supportive healthcare policies to effectively expand telemedicine services. Future work should focus on developing and evaluating tailored interventions to assess the effectiveness of hybrid donor evaluation models.
The Telemedicine Workgroup at the American Society of Transplantation Living Donor Community of Practice (AST LDCOP).
[1] Living donation
[2] Kidney donors
[3] Donor Selection
[4] Kidney Transplantation
[5] Telehealth
[6] Healthcare Access