Turning potential into hope: How PPDDP is transforming organ donation in Iran
Ehsan Radi1, Katayoun Najafizadeh1,2, Omid Ghobadi1.
1Organ donation, Iranian Research Center of Organ Donation, Tehran, Iran; 2Organ donation, Shahid Beheshti University of Medical Science , Tehran, Iran
Introduction: Extensive variability exists on how to approach the identification and referral (ID&R) of brain-dead organ donors (OD), leading to variations in the number of procured organs worldwide.
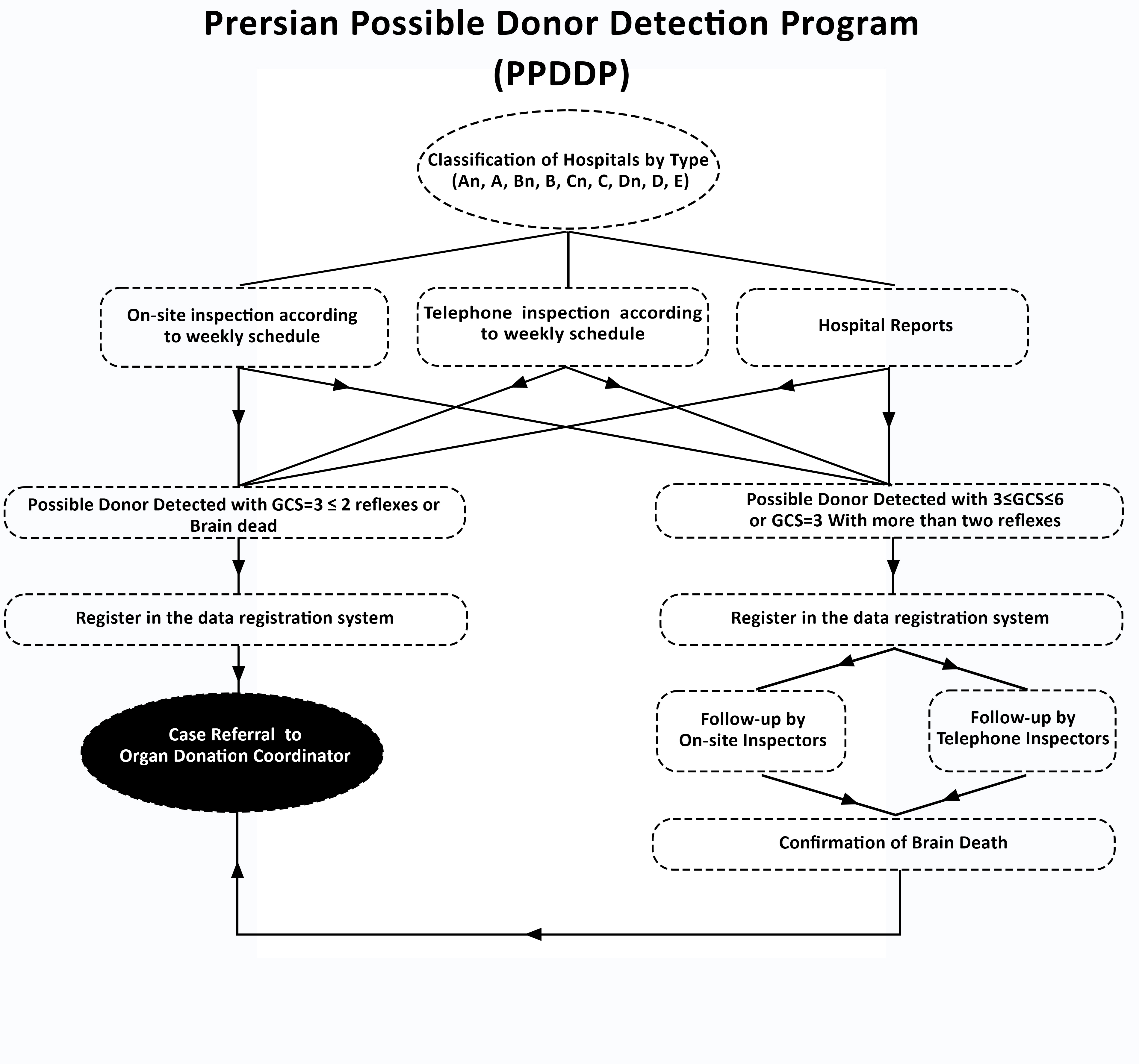
Methods: The present intervention was conducted through the OPUs of Shahid Beheshti University of Medical Sciences in Tehran which is responsible for managing the 113 included hospitals. In our new method aimed at maximizing the detection of brain-dead donors across all affiliated hospitals without requiring numerous in-hospital coordinators, we established on-site, telephone detectors, and enlisted some hospital staff as reporters. A monthly comprehensive schedule was devised for hospital assessments, aiming to optimize donor detection for both on-site and telephone detectors. This schedule factored in variables like the number of ICU beds and the presence or absence of neurosurgery/neurology wards. Furthermore, telephone and on-site inspections were coordinated to minimize the time gap between assessments. All of the detected possible ODs without a known contraindication for organ donation were evaluated by detectors to be categorized based on their prognosis. three separate categories of the now potential ODs (PODs) were defined: (I) PODs with Glasgow Coma Scale (GCS) scores of 4, 5, or 6, (II) PODs with a GCS score of 3 and a low clinical suspicion of brain death (at least one inconsistency with brain death diagnosis). Category II cases were further subdivided into two subcategories: Category IIA, comprising PODs with three or more brainstem reflexes, and Category IIB, comprising PODs with less than three brainstem reflexes, and (III) PODs with a GCS score of 3 and a high clinical suspicion of brain death (no detected inconsistencies with brain death diagnosis). All identified cases were recorded on the project's designated website (Figure 1).
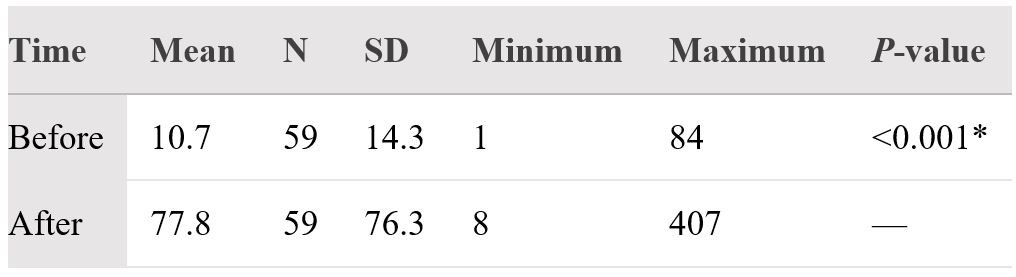
Results: The number of detected cases before and after the PPDDP method's implementation was compared using data gathered from 59 hospitals. The total number of detections based on GCS<7 before and after the intervention was recorded as 633 and 4589 respectively, indicating a more than seven-fold improvement (Figure 2).
One of the study's most significant takeaways from the results is that 49% of those who are eligible donor organs come from non-brain death follow-up. In other words, among cases who were eligible donors, there was no significant difference between the number of brain death and non-brain death. This issue indicates the need to use an efficient detection program to identify possible donors in all medical centers.
Discussion: The study's findings indicate that the PPDDP identification program's implementation significantly increases the number of eligible cases. PPDDP implementation is ten times less expensive than the active detection model. In terms of ultimate efficiency, this cost decrease is not much different from the Active D. approach.
[1] Possible Donor
[2] Organ Donation
[3] Donor Detection
[4] Eligible Donor