Insights from refusal patterns for deceased donor kidney offers
Grace Guan1, Sanjit Neelam1, Joachim Studnia1, Xingxing S Cheng2, Marc L Melcher3, Michael A Rees4, Alvin E Roth5, Paulo Somaini6, Itai Ashlagi1.
1Management Science and Engineering, Stanford University, Stanford, CA, United States; 2Nephrology, Stanford University, Stanford, CA, United States; 3Surgery, Stanford University, Stanford, CA, United States; 4University of Toledo, Toledo, OH, United States; 5Economics, Stanford University, Stanford, CA, United States; 6Graduate School of Business, Stanford University, Stanford, CA, United States
Introduction: The likelihood that a deceased donor kidney will be utilized evolves during the allocation process. Transplant centers can either decline a deceased donor kidney offer for a single patient or for multiple patients at the same time. We hypothesized that refusals for a single patient indicate issues with individual patients, whereas simultaneous refusals for multiple patients indicate issues with organ quality. Uncovering which refusals are based on organ quality early (e.g., before cross-clamp) can help identify organs at high risk of nonuse and determine candidacy for accelerated placement.
Methods: We conducted a descriptive analysis of offer refusal patterns between January 1, 2022 and December 31, 2023 using Organ Procurement and Transplantation Network data. We aggregated refusals at the same timestamp by a transplant center, and we defined a multi-patient refusal as a situation where at least two patients from a transplant center refused the organ at the same time. We analyzed the refusal codes associated with single- and multi-patient refusals and the nonutilization rate after receiving single- and multi-patient refusals by cross-clamp.
Results: There were 880,647 single or multi-patient refusals for donors in our cohort, of which 69.1% (608,279) were multi-patient and 30.9% (272,368) were single-patient, and 230,380 (25.6%) occurred prior to cross-clamp. Of the multi-patient refusals, 98% had the same refusal code reported for all patients refused simultaneously. Patient-related refusal reasons were more commonly single-patient refusals, whereas organ-related refusal reasons were more commonly multi-patient refusals. The likelihood of nonutilization increased with the number of centers issuing multi-patient refusals before clamping, even after controlling for KDPI (Figure 1). Conversely, the likelihood of nonutilization decreased as the number of single-patient refusals increased.
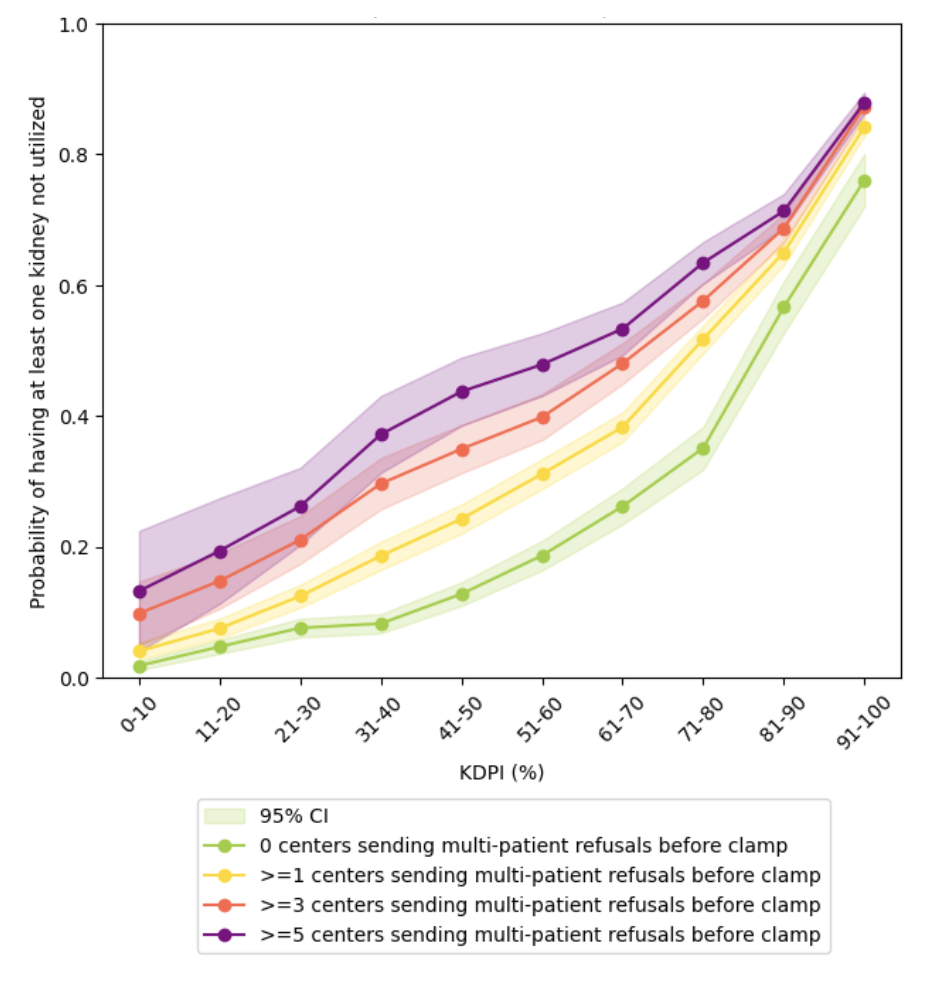
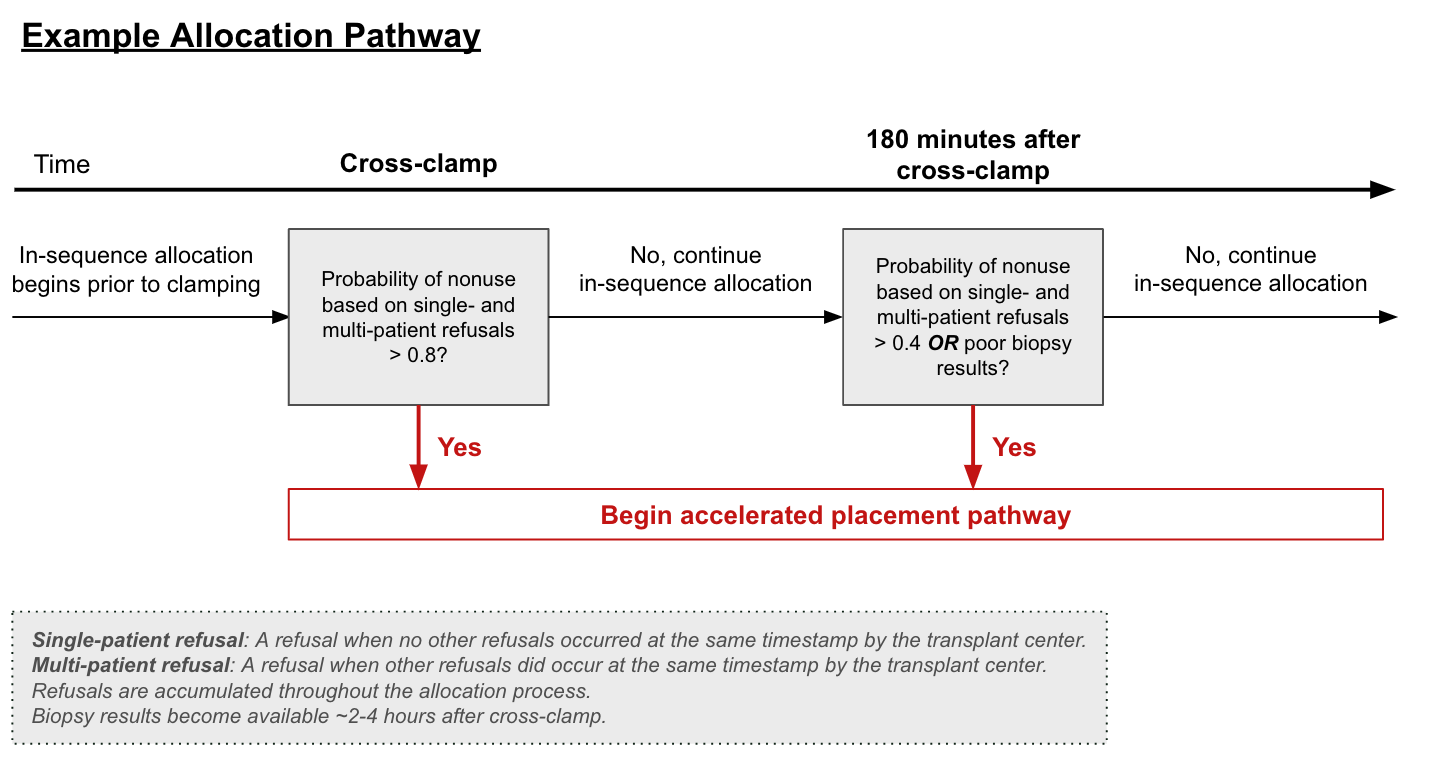
Conclusions: There could be many valid clinical concerns regarding a donor that are not represented in the KDPI or any other risk index based on registry data. These include the concerns for infection or malignancy, anatomical or surgical aberrations, procurement issues, and other medical factors. Multi-patient refusals, even those prior to cross-clamp, can identify hard-to-place organs reliably regardless of the specific reason and without need for additional data collection, making it a highly promising tool for developing accelerated pathways of kidney allocation (example given in Figure 2). For example, the historical probability of nonutilization based on single- and multi-patient refusals can be calculated and used to determine when to begin an accelerated placement pathway. The threshold for these policies can be adjusted based on organ-specific factors, as well as cold ischemia time. The time of decision making is flexible and can be performed at any point during the allocation process.
[1] Organ Procurement and Transplantation Network
[2] Deceased Donor Kidney
[3] Organ allocation
[4] Organ utilization