Temporal trends in organ donation consent rates in New South Wales, Australia
Rachel B Cutting1, James A Hedley1, Nicole L De La Mata1, Kate Wyburn2,3, Michael J O'Leary4,5, Angela C Webster1,6.
1Faculty of Medicine and Health, Sydney School of Public Health, University of Sydney, Sydney, Australia; 2Sydney Medical School, University of Sydney, Sydney, Australia; 3Renal Unit, Royal Prince Alfred Hospital, Sydney Local Health District, Sydney, Australia; 4NSW Organ and Tissue Donation Service, Kogarah, Australia; 5Intensive Care Service, Royal Prince Alfred Hospital, Sydney, Australia; 6Westmead Applied Research Centre, Faculty of Medicine and Health, University of Sydney , Westmead , Australia
Aims: Efforts to improve next-of-kin consent are important in increasing the number of deceased organ donors for transplantation. We examined temporal trends in next-of-kin consent rates in NSW, Australia.
Method: Cohort study of all people considered for deceased organ donation in NSW 2010-2023, using the Organ Referral Characterisation Database (ORCHARD). We used logistic regression to examine trends in consent rates over time, adjusted for donor factors and the COVID-19 pandemic (2020-2023) and hospital site. Donor factors included age, sex, ethnicity, religion, socioeconomic deprivation, remoteness, and comorbidities.
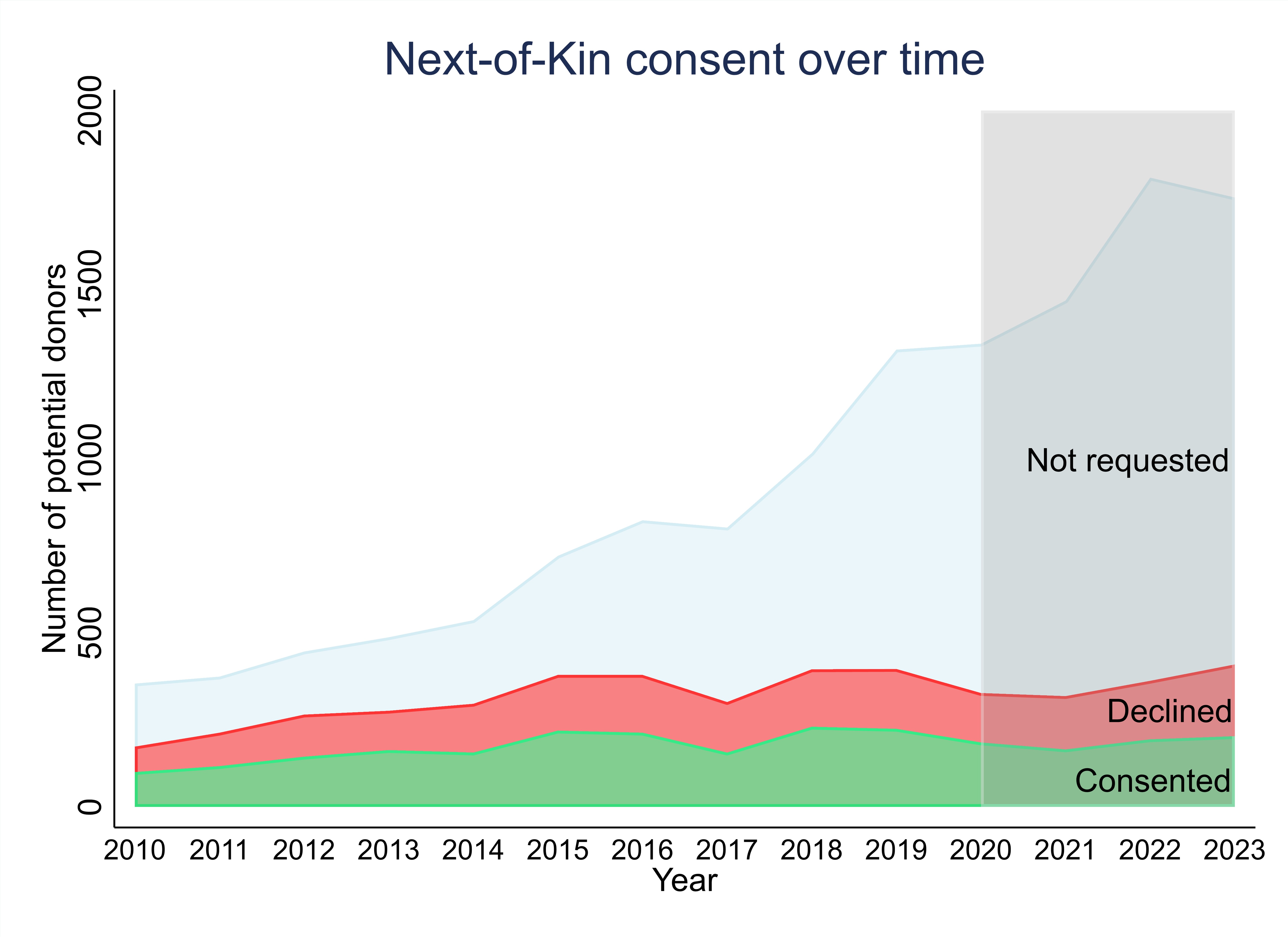
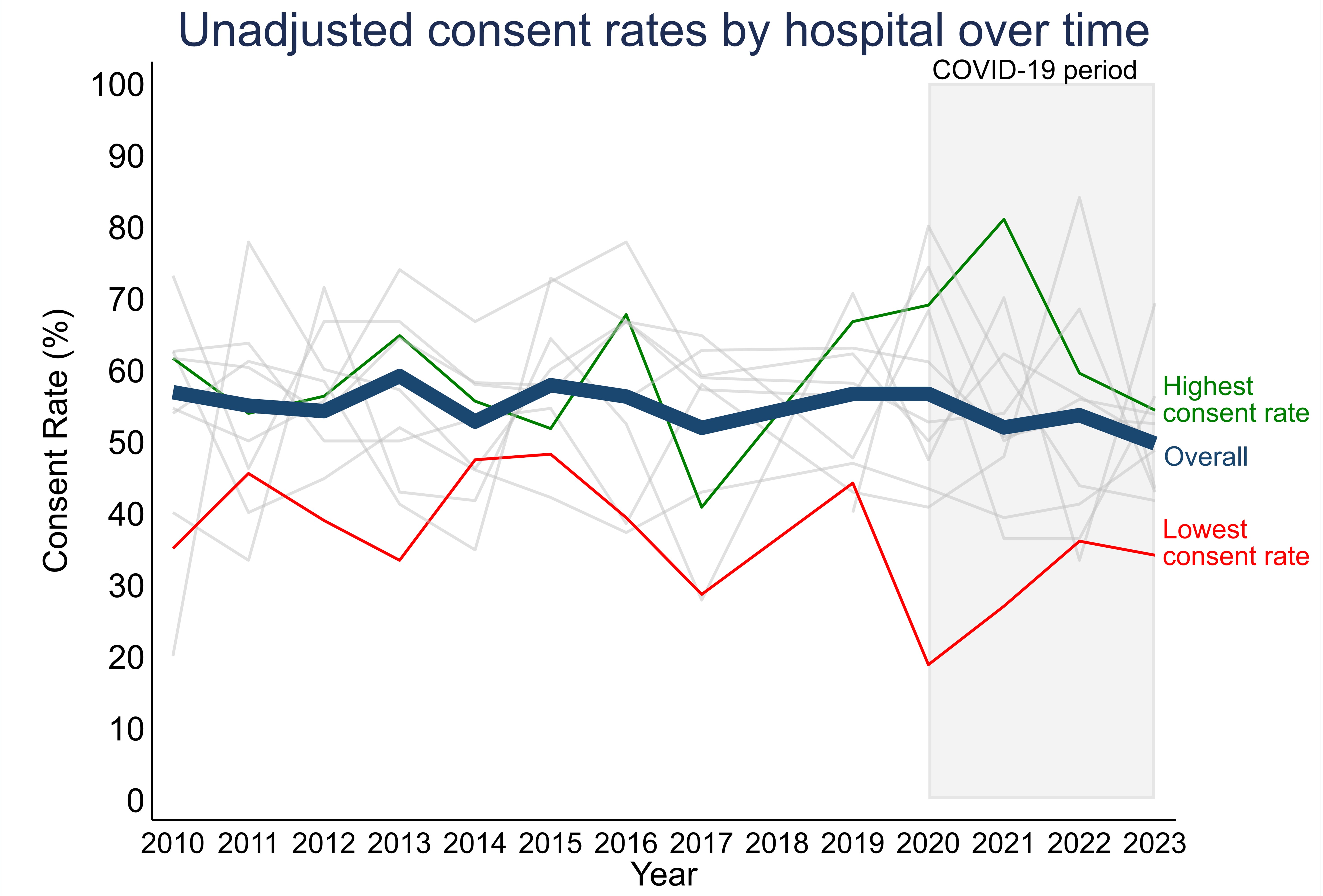
Results: Of 13,213 potential deceased donors, next-of-kin consent was requested for 4,484 (34%), of whom 2,464 (55%) received consent and 2,020 (45%) were declined. Potential donors increased over time likely due to the Australian Government’s 2009 national program, but consent rates did not (Figure 1a). Overall, the adjusted consent rate decreased over time pre-pandemic (annual OR 0.90, 95%CI: 0.86-0.94, p<0.001) but remained steady during the pandemic (annual OR 0.95, 95%CI: 0.85-1.07, p=0.4). There were differences in consent rate by age, ethnicity, religion and socioeconomic status (all p<0.001). On average, hospital specific consent rates remained steady over time (annual IRR 0.99, 95%CI: 0.98-1.00 p>0.05, Figure 1b) but differed by site (p<0.001).
Conclusion: Despite increases in potential donors considered, the number of cases approached for next-of-kin consent has remained stable overall and by hospital. Consent rates are similarly unchanged overtime and no evidence the pandemic impacted agreements. Further investigation is needed to more granularly explore case mix of potential donors considered and approached over time.