Clinical risk aversion of potential deceased kidney donors forgone for biovigilance concerns: A data-linkage study
Brenda Rosales1, Rachel Davies1, James A Hedley1, Nicole De La Mata1, Melanie Wyld1, Elena Cavazzoni2, Kate Wyburn3,4, Patrick J Kelly1, Angela C Webster1,5.
1Centre for Organ Donation Evidence, Sydney School of Public Health, The University of Sydney, Sydney, Australia; 2NSW Organ and Tissue Donation Service, New South Wales Health, Sydney, Australia; 3Central Clinical School, Faculty of Medicine and Health, The University of Sydney, Sydney, Australia; 4Renal Medicine & Transplant, Royal Prince Alfred Hospital, Sydney, Australia; 5Westmead Applied Research Centre, Westmead Hospital, Sydney, Australia
Centre for Organ Donation Evidence.
Introduction: Biovigilance risk from cancer or infection in potential deceased organ donors varies and can challenge decision-making. We sought to estimate donation and transplant gains achievable from increasing clinical consistency in potential donor medical suitability decisions.
Methods: Using current Australian and New Zealand clinical guidelines we interrogated a data-linked biovigilance register, to identify and describe potential kidney donors deemed not suitable for transplantation due to a higher than baseline but still guideline-acceptable risk of cancer and/or infection (clinical risk aversion) in NSW, Australia, 2015-2022. We estimated gain in donors per million population (pmp) should these donors have been accepted.
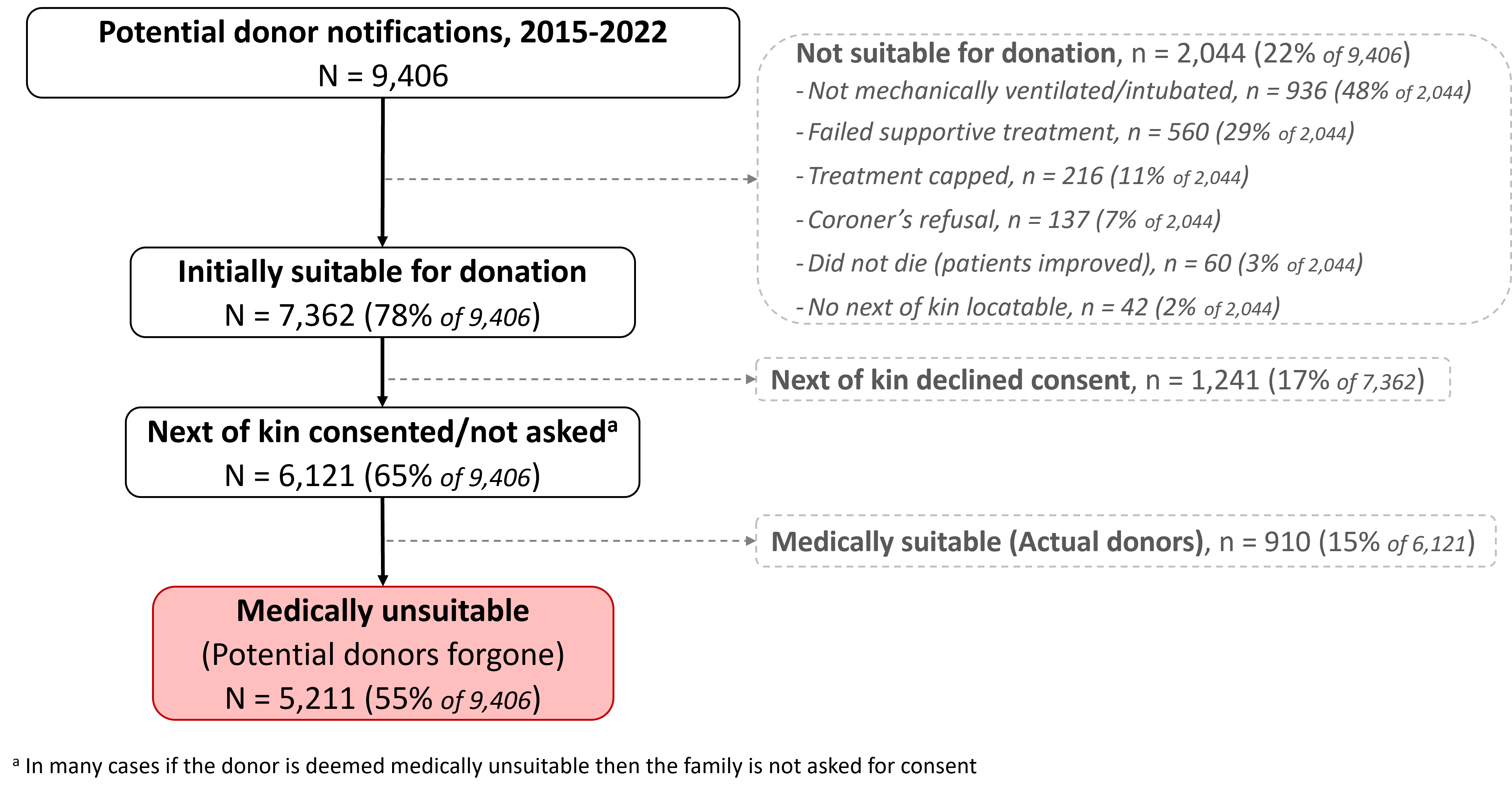
Results: Of 5,211 potential donors deemed not medically suitable and included in our cohort (Figure 1), 674 (13%) were forgone for clinical risk aversion, an average of 84 (1.6%) donors annually.
Of these donors forgone for risk aversion, 317 (49%) had increased risk behaviours for blood-borne viruses but had either no virus, historic Hepatitis B or historic or active Hepatitis C, 539 (20%) had an historic cancer diagnosis of minimum to low transmission risk, and 328 (49%) had a current other treatable infection with no evidence of sepsis or organ damage. Donors forgone for risk aversion were majority male (62%), over 55 years (75%), with one or more comorbidities (85%).
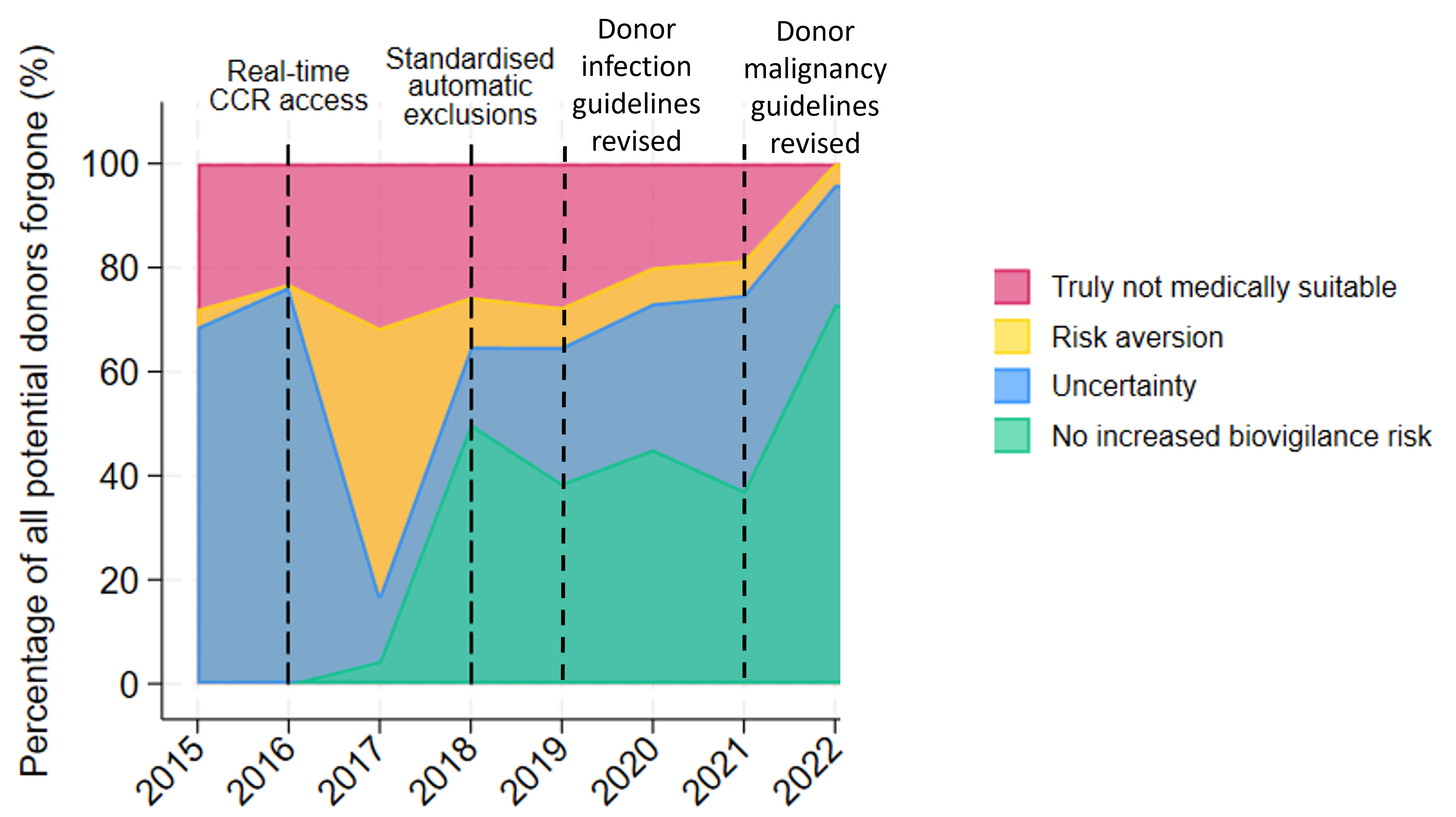
The proportion of potential donors forgone for risk aversion increased to over 40% in 2017, after the introduction of real-time access to centralised cancer records (CCR) (Figure 2). Clinical risk aversion fell again after donor infection and malignancy transmission guidelines were revised in 2019 and 2021. In 2022, 4% of potential donors forgone were due to clinical risk aversion.
Accepting donors deemed not medically suitable and forgone for clinical risk aversion could have increased annual NSW donation rates by up to 4.9 to 9.9 donors pmp, assuming 55% and 100% donor consent rates, respectively. In particular, donors with current Hepatitis C would require the recipient's informed consent and treatment.
Conclusion: Clearer guidelines and organ donation system changes decreased the proportion of donors forgone for clinical risk aversion. However, there remains significant clinical risk aversion for many donors with biovigilance concerns who could have safely donated. Accepting these donors could increase donation rates from 17.5pmp in NSW to 22.4pmp, significantly impacting Australia's rates overall. Challenging risk-averse decisions could provide viable transplant opportunities nationwide.
With thanks to the Office of the Chair, NSW Health; Kidney Health Australia; New South Wales Organ and Tissue Donation Service; Australian and New Zealand Dialysis and Transplant Registry; Australian and New Zealand Liver Transplant Registry; Australian and New Zealand Islet and Pancreas Transplant Registry; Australian and New Zealand Cardiothoracic Transplant Registry.
[1] Biovigilance
[2] Medical suitability
[3] Population study
[4] Solid organ donation
[5] Donation rates
[6] Disease transmission