Prospective cohort profile of transplantation recipients and donors aiming to identify biopsychosocial markers of postoperative outcomes
Hyejin Kim1,2, Jieun Noh2, Yoonjae Cha1, Eunhye Kim1, Juhan Lee4, Sun Jae Jung1,2,3.
1Department of Preventive Medicine, Yonsei University College of Medicine, Seoul, Korea; 2Department of Public Health, Graduate School, Yonsei University, Seoul, Korea; 3Institute for Innovation in Digital Healthcare, Yonsei University, Seoul, Korea; 4Department of Surgery, The Research Institute for Transplantation, Yonsei University College of Medicine, Seoul, Korea
In South Korea, kidney and liver transplantation are primary treatments for end-stage organ failure, with a substantial proportion of procedures involving living donors. Although recent studies suggest that psychological resilience is associated with physical health, particularly immune function, with resilient individuals showing better recovery from inflammation, little is known about how resilience or mental health before and during treatment affects immune reconstitution and outcomes in donors and recipients. Therefore, the Mental health, Resilience and Immune system in Transplantation recipients and donors (MeRIT) cohort was established to prospectively collect high-quality data on multidimensional indicators of postoperative outcomes in kidney and liver transplantation.
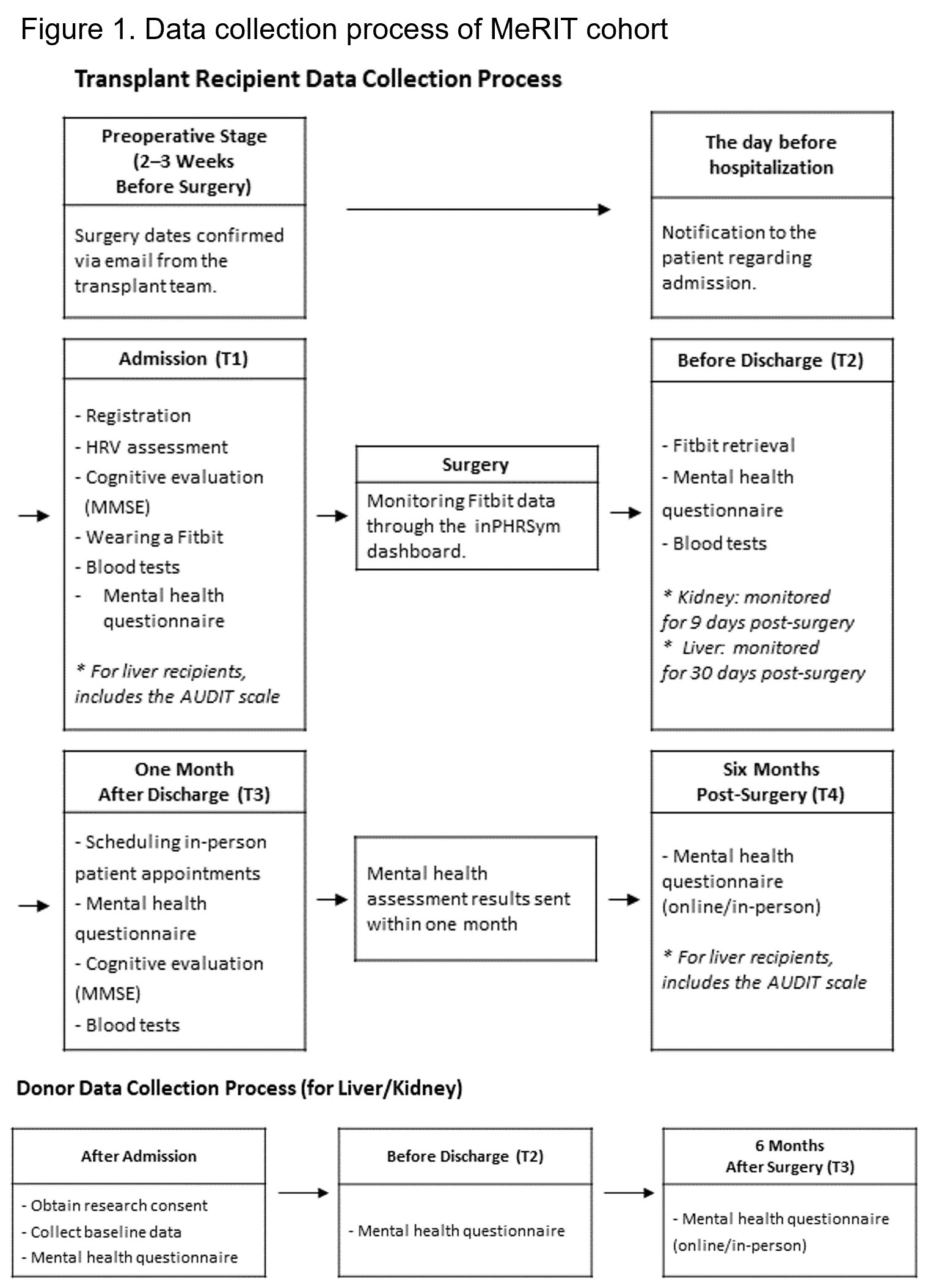
This project is led by a multidisciplinary team that includes professionals from psychiatric epidemiology, transplant surgery, laboratory medicine, and nursing. Data collection began in November 2024 and is expected to continue until December 2026 at Severance Hospital, a single private tertiary hospital in Seoul, South Korea. During pre-transplant consultations, kidney and liver transplant donors and recipients aged 18 or older are invited to participate. The target sample size includes 200 kidney and 100 liver transplant donor–recipient pairs. For recipients, assessments were conducted at four time points (see Figure 1): hospital admission, discharge, 1-month post-transplant, and 6-month follow-up. For donors, assessments occurred at admission, discharge, and 6 months post-discharge. Most psychological and psychosocial variables were measured at each time point using validated instruments. An autonomic nervous system testing device was used to assess heart rate variability indicating psychophysiological stress of participants. Recipient blood samples will be used for future analyses of complete blood count, cytokine levels, and proteomic profiles. Wearable devices were used during hospitalization to continuously monitor physical activity, sleep, and heart rate.
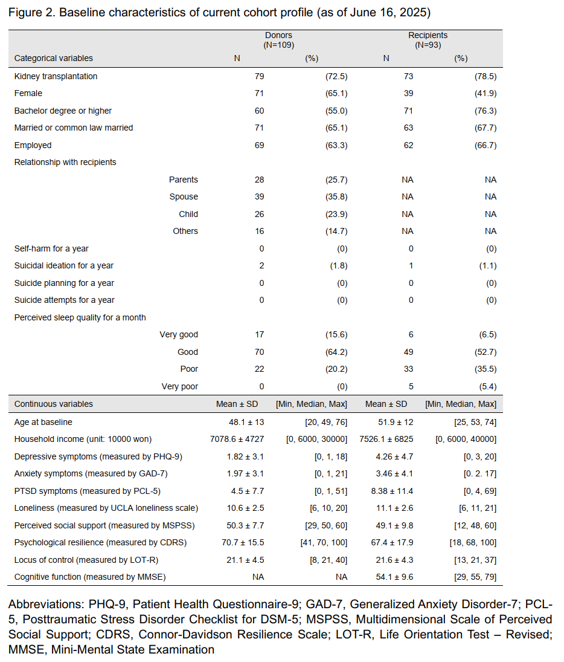
As of June 16, 2025, a total of 109 donors and 93 recipients had been recruited, with 73% of the donors and 79% of the recipients being kidney donors and recipients, respectively (see Figure 2). Most donors and recipients were immediate family members. While the majority of donors were female, recipients were predominantly male and tended to be older. Compared to donors, recipients exhibited greater levels of psychological symptoms, including depression, anxiety, posttraumatic stress, and loneliness. However, the two groups showed similar levels across positive psychological indicators, including perceived social support, resilience, and locus of control. We plan to continue building this prospective cohort until December 2026 and to conduct longitudinal analyses after further enrollment.
This research was supported by a grant of the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare, Republic of Korea (grant number: RS-2024-00440320).
[1] Cohort profile
[2] Prospective cohort
[3] Mental health
[4] Resilience
[5] Kidney transplantation
[6] Liver transplantation
[7] Postoperative outcome