Early surgical experience and learning curve of robot-assisted donor nephrectomy by a junior surgeon: A propensity score-matched comparison with laparoscopic approach
Ara Cho1, Jongwon Ha1, Sangil Min1.
1Transplantation and Vascular Surgery, Seoul National University Hospital, Seoul, Korea
Background: Robot-assisted donor nephrectomy (RDN) is increasingly used in living kidney donation as a minimally invasive alternative to conventional approaches. However, evidence on its implementation during the early surgical training phase remains limited. This study aimed to evaluate the early surgical experience and learning curve of RDN performed by a single junior surgeon at a high-volume transplant center, with outcomes compared to laparoscopic donor nephrectomy (LDN) using a matched cohort.
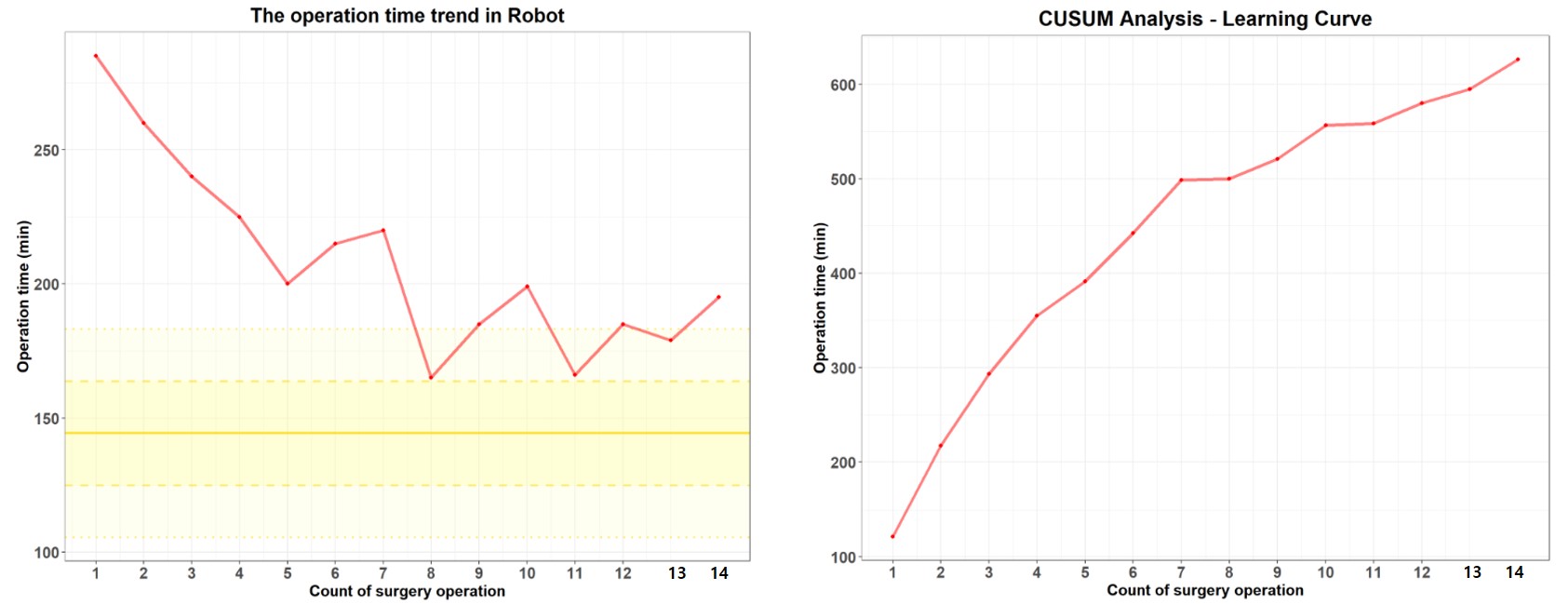
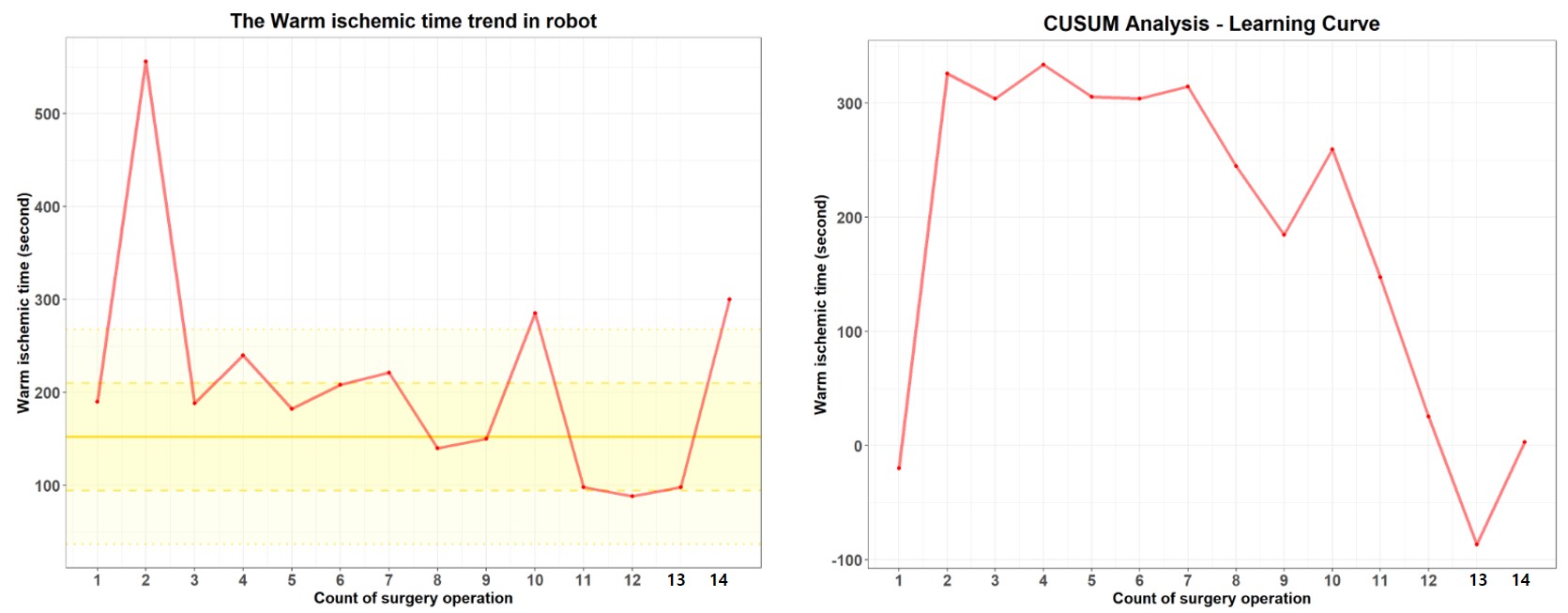
Methods: We retrospectively reviewed 14 consecutive RDNs performed by a junior surgeon. For comparison, 14 LDN cases were selected from a total of 98 laparoscopic nephrectomies performed during the same period using 1:1 propensity score matching based on donor characteristics (BMI, renal vascular anatomy, and laterality). Perioperative parameters—including operative time, warm ischemic time (WIT), estimated blood loss, length of hospital stay, and postoperative complications—were compared. Learning trends were assessed using cumulative sum (CUSUM) analysis of operative time and WIT.
Results: The mean operative time was significantly longer in the RDN group compared to the matched LDN group (208.5 ± 35.0 minutes vs. 144.4 ± 19.4 minutes, p < 0.001). Mean WIT was also longer in RDN cases (210.3 ± 119.2 seconds vs. 152.3 ± 57.8 seconds), though not statistically significant (p = 0.118). No intraoperative complications or conversions to open surgery occurred in either group. All donors were discharged without major morbidity. Postoperative renal function was comparable between groups. CUSUM analysis showed a gradual decline in operative time and stabilization of WIT, suggesting a continuous improvement without abrupt changes.
Conclusions: Robot-assisted donor nephrectomy can be safely initiated by junior surgeons under appropriate training. While RDN initially required longer operative and ischemic times compared to laparoscopic cases, outcomes improved with experience and remained within acceptable clinical ranges. These findings support the feasibility of incorporating RDN into transplant training and highlight the role of institutional support in its safe implementation.
[1] Robot-assisted donor nephrectomy
[2] Learning curve
[3] Living kidney donation
[4] CUSUM analysis
[5] Junior surgeon