Staff awareness and attitudes towards organ and tissue donation in transplanting centres vs. non-transplanting hospitals - is there a difference?
Emiliano Mazzaretto1, Alice Workman1, Matthew Harrison1, Kim O'Connel1, Helen Foley1, Kathryn Cannon1, Robin Prescott1.
1Organ Donation and Transplantation, NHS Blood and transplant, London, United Kingdom
Introduction: This staff survey investigated differences in awareness and attitudes toward organ and tissue donation between healthcare professionals (HCPs) in transplanting and non-transplanting hospitals in North and North-West London. Given the vital role of ICU and ED staff in initiating referrals, understanding barriers and educational gaps is essential to improving organ donation rates. Despite the introduction of deemed consent legislation in England in 2020, national consent rates have not increased significantly, partly due to limited staff and public awareness; an issue exacerbated by the COVID-19 pandemic.
Methods: An anonymous survey, developed by Specialist Nurses in Organ Donation (SNODs), was distributed to ICU and ED staff at two transplanting and two non-transplanting hospitals. The survey included demographic data and questions on attitudes, awareness, and confidence in the donation referral process, using both open-ended and Likert-scale formats. Participation did not require ethical approval as it was classified as a service evaluation. Data were compared across the two hospital groups to identify trends and differences.
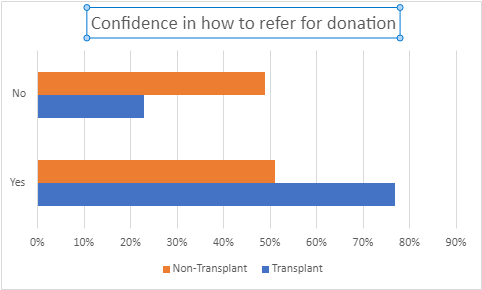
Results: Seventy-three responses were collected, with 75% from non-transplanting centres. ED staff represented only 10% of total responses. Transplanting centre staff were marginally younger and reported greater exposure to organ donation education (83% vs. 53%) and higher confidence in referring patients (77% vs. 51%).
However, awareness of deemed consent legislation was comparable (72% in transplanting vs. 67% in non-transplanting centres). Both groups showed strong support for organ donation and recognized its benefits. Free-text responses emphasized the importance of continued education and the positive influence of SNODs.
Conclusions: Although transplanting hospitals demonstrated slightly higher awareness and confidence in organ donation practices, the differences were modest. Low response rates, especially from transplanting centres, limit the generalizability of findings. Key recommendations include increasing teaching in non-transplanting centres, implementing a Link Nurse programme to disseminate knowledge, and developing clear, locally tailored referral triggers aligned with national guidelines. Greater consistency in education and awareness initiatives is essential to ensure organ and tissue donation is effectively integrated into end-of-life care pathways.
[1] Organ Donation
[2] staff attitudes
[3] transplanting centres
[4] non-transplanting hospitals