Impact of a standardized anesthesia protocol on safety and quality outcomes in 1289 cases undergoing robotic donor hepatectomy: A single center experience
Amer Majeed1,2, Arshad Mahmood1, Dimitri A Raptis1, Dieter C Broering1,2.
1Abdominal Transplant and Hepatobiliary Surgery, King Faisal Specialist Hospital & Research Centre, Riyadh, Saudi Arabia; 2College of Medicine, Alfaisal University, Riyadh, Saudi Arabia
Introduction: Robotic surgery for Living Donor Hepatectomy (LDH) has a potential to reduce morbidity and offer faster recovery, less pain, shorter ICU and hospital stay, and greater patient satisfaction from smaller incisions [Kakos 2023].
It poses unique anesthetic challenges, such as: increased duration of the procedure, hemodynamic effects of pneumoperitoneum and reverse Trendelenburg position, restrictive fluid management to avoid liver congestion, etc.; the lack of evidence base makes calibration of anesthetic management difficult.
Robotic LDH started in our institution in 2018 and became our standard of care in 2021 [Schulze 2022]. We have evaluated the impact of our standardized anesthesia protocol on the safety and quality outcomes.
Material and methods: The data on all the LDH cases from our institution's LT registry (2011 – 2024) were analyzed.
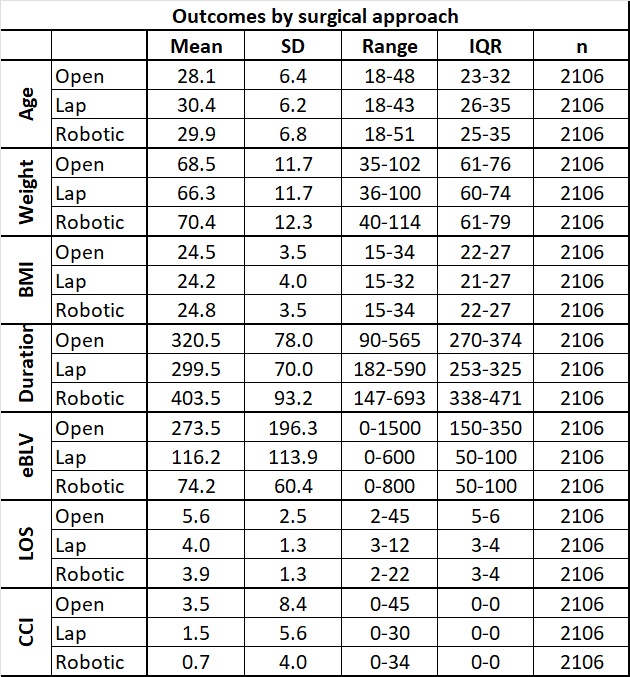
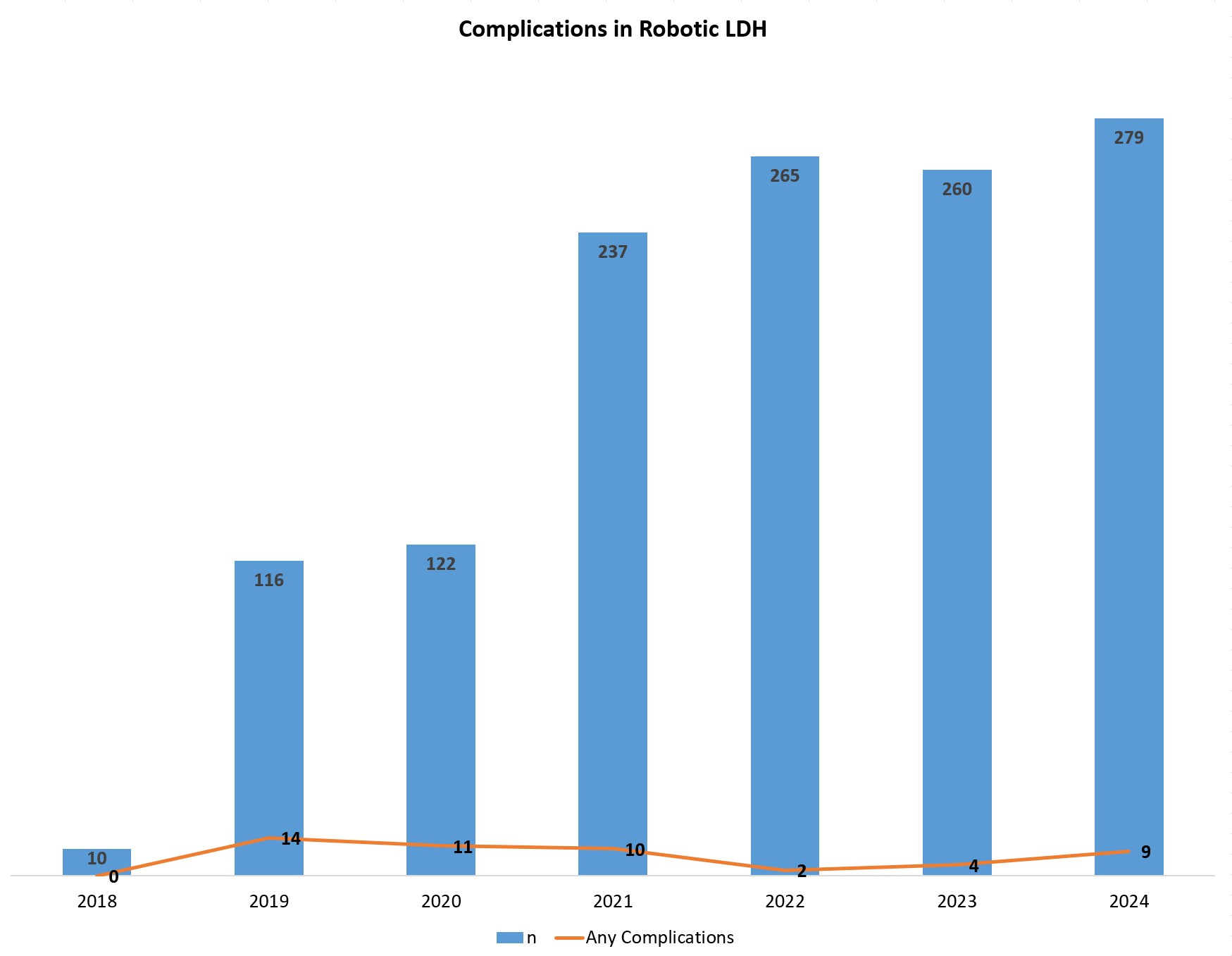
Results: The LDH (n=2106) surgical approach was Open (n=646), Laparoscopic (n=133), robotic (n=1289), laparoscopic assisted (n=32) or Robotic assisted (n=6); only 6 cases were converted to open (robotic=2). Right lobe was taken robotically in 609, Left in 296, and Left Lateral (LL) in 384 cases. A total of 188 complications of any severity were recorded in 165 patients, of which only 7 were major (Clavein Dindo grade ≥3a); Comprehensive Complication Index (CCI®) scores (n=165, 7.8%, range 0 – 44.8,) were lower (0 – 33.7) and less frequent (n=46, 3.5%) in the Robotic group and the Left Lobe. Robotic surgery took an average of extra 103 or 84 minutes from Open or Laparoscopic approaches; however, the lower mean blood loss by 210 mls or 43 mls, respectively. Similarly, they discharged from hospital on average 1.69 or 0.48 days sooner than the Open or Laparoscopic groups.
Figure 1 summarizes the results; Figure 2 depicts timeline of Robotic LDH complications.
Conclusion: Informed by the local clinical governance systems (incident reports, morbidity reviews, audits, etc.) we standardized our anesthetic protocol in 2018; the key management points include large IV access, a radial arterial line and a single lumen 4 French catheter (Leadercath, Vygon, France) in right internal jugular vein, sevoflurane maintenance, IV infusions of Fentanyl, myorelaxant, and phenylephrine, started before positioning, restrictive fluid therapy until splitting of the graft is completed (guided by trends instead of absolute values in SPV and PPV), frusemide 0.1-0.2 mg/kg bolus if opening CVP >10 cm of H2O, and target abdominal pressure <15 cm of H2O. All patients are extubated, and the CVC and orogastric tube are removed at the end of surgery. As reported before, within the first 48 hours post-operatively 85% patients have mild (Visual Analog Score ≤3/10) pain, without PCA [Majeed 2025].
Robotic LDH appears to be safer and with better outcomes. Meticulously tailored standardized Anesthesia management protocol is crucial in achieving these outcomes.
[1] Robotic surgery
[2] minimally invasive surgery
[3] donor hepatectomy
[4] anesthesia