Predictive role of kidney volume indexed to BSA on post-donation kidney function in living kidney donors
Kyowon Lee1, Kyungho Lee3, Sunghae Park 1, Hye Ryoun Jang3, Jea Berm Park 1, Kyung A Kang 4, Min Jung Kim 2.
1Surgery , Samsung Medical Center, Seoul, Korea; 2Surgery , Seoul Medical Center , Seoul, Korea; 3Medicine , Samsung Medical Center, Seoul, Korea; 4Radiology, Samsung Medical Center, Seoul, Korea
Objective: To determine whether preoperative kidney volume measured on CT independently predicts post-donation chronic kidney disease (CKD) in living kidney donors, and whether it improves risk prediction beyond clinical variables.
Methods: This retrospective study included 410 living kidney donors (mean age, 47.6 ± 12 years) who underwent donor nephrectomy from 2016 to 2021 and had follow-up estimated glomerular filtration rate (eGFR) data. Cortical and whole kidney volumes (CV and WV) of the remnant kidney were measured from preoperative CT and normalized to body surface area (BSA). The primary outcome was CKD, defined as eGFR <60 mL/min/1.73 m² at 1- and 5-years post-donation. Associations between kidney volume and post-donation renal function were assessed using Pearson correlation, logistic regression (1-year CKD), and Cox regression (5-year CKD). Model performance was evaluated using AUC and integrated discrimination improvement (IDI).
Results: Lower WV/BSA was independently associated with increased CKD risk at 1 year (OR, 0.93; p=0.0002) and 5 years (HR, 0.95; p<0.0001). Age, BMI, and baseline eGFR were also significant predictors (all p<0.05). WV/BSA correlated better with postdonation eGFR than unadjusted volumes.
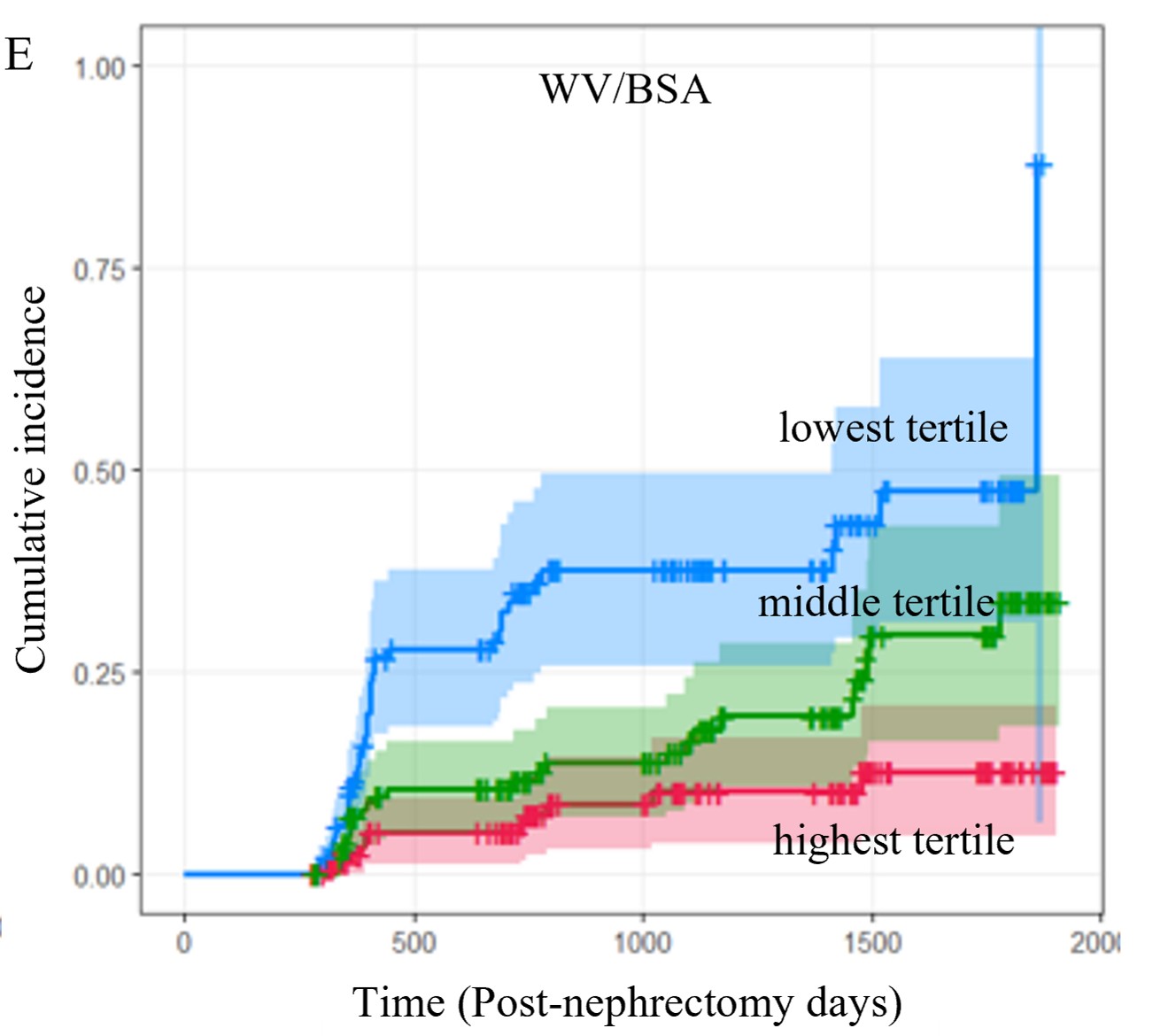
Adding WV/BSA to a clinical model improved fit (R²: 0.481 vs. 0.428) and discrimination (IDI: 0.053, p=0.008). Predictive association was most pronounced in donors with baseline eGFR <90 mL/min/1.73 m². CV/BSA was not a significant predictor in multivariable analysis.
Conclusion: Preoperative whole kidney volume indexed to BSA is an independent predictor of post-donation CKD and improves risk stratification beyond clinical factors.
[1] Chronic Kidney Disease
[2] Kidney Volume
[3] Computed
Tomography Angiography
[4] Living Kidney Donors