The predictive value of double negative T cell migration for transplant rejection and early death after lung transplantation
Fan Xu1,2, Li Ke2, Min Zhou1.
1Department of Critical Care Medicine, The First Affiliated Hospital of University of Science and Technology of China (USTC), Hefei, People's Republic of China; 2Department of thoracic surgery, The First Affiliated Hospital of University of Science and Technology of China (USTC), Hefei, People's Republic of China
Introduction: Lung transplantation is the ultimate treatment intervention for end-stage lung diseases; However, compared to other solid organ transplants, the long-term survival rate of lung transplant recipients is still not optimal, mainly due to mortality related to lung transplant dysfunction [1-2]. The current gold standard monitoring methods, such as bronchial biopsy, are invasive and lack sensitivity to early transplant rejection and death detection [3]. It is crucial to note that the pathophysiological basis linking the progression of allogeneic rejection to early post transplant mortality, particularly early post transplant immune rejection and hypoxia driven immune dysregulation, has yet to be well described [1-3]. Previous studies have found that double negative T cells are regulatory T cells that maintains immune homeostasis [4]. This study integrated flow cytometry and multi omics to investigate the effects of DNT cells on 28 day mortality and pulmonary dysfunction caused by allogeneic rejection after lung transplantation.
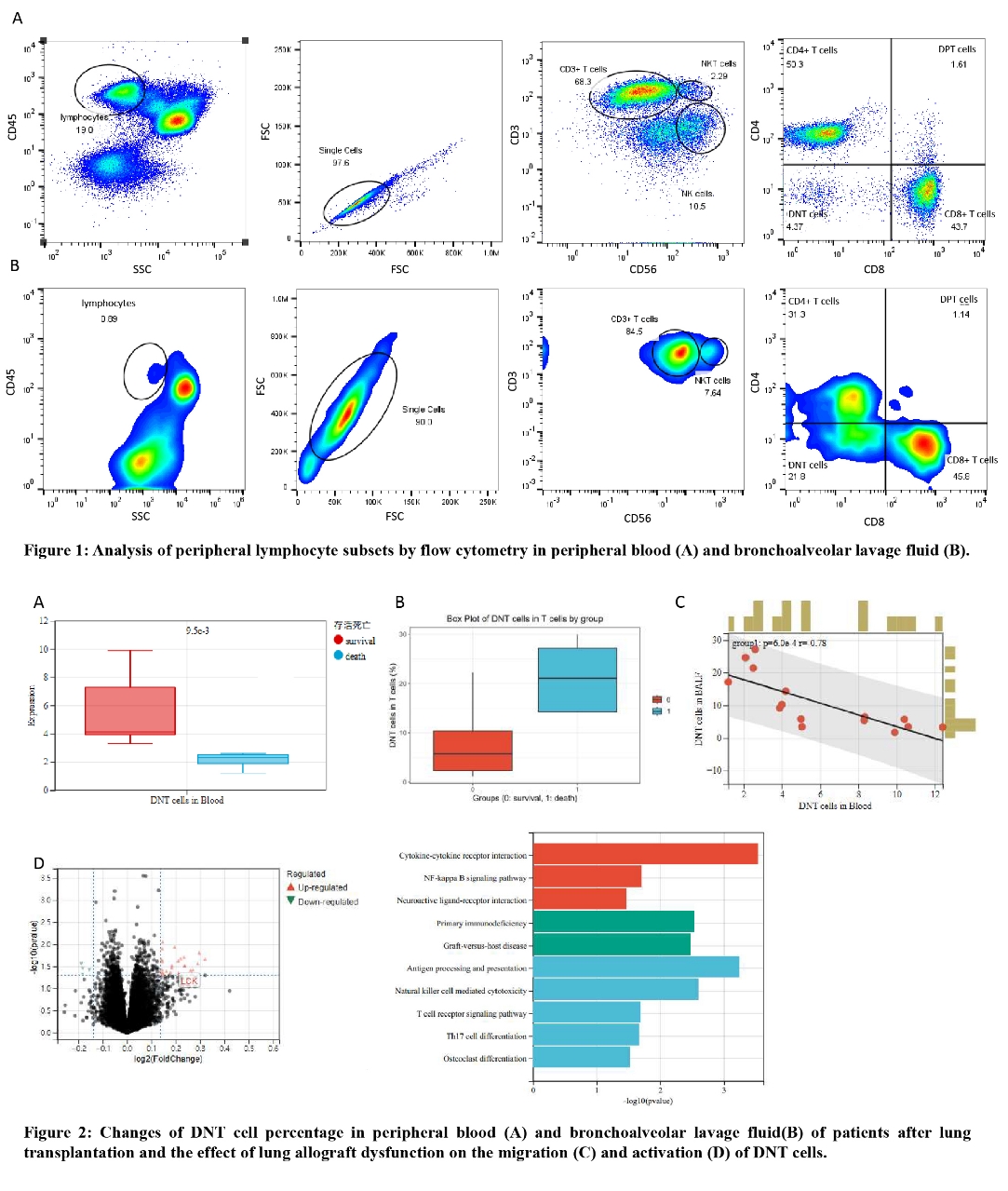
Methods: Flow cytometry was performed on peripheral blood and bronchoalveolar lavage fluid (BALF) from 17 recipients within 72 hours after lung transplantation using panel targeting surface markers to profile T cells and NK cells, and evaluate immune functions (Figure1.1). Two external transcriptomic datasets (N=16) were analyzed to explore the relationship between DNT cells and chronic lung allograft dysfunction[5]. Murine left lung scRNA-seq under normobaric hypoxia/normoxia was conducted to elucidate hypoxia's role in immune cell differentiation.
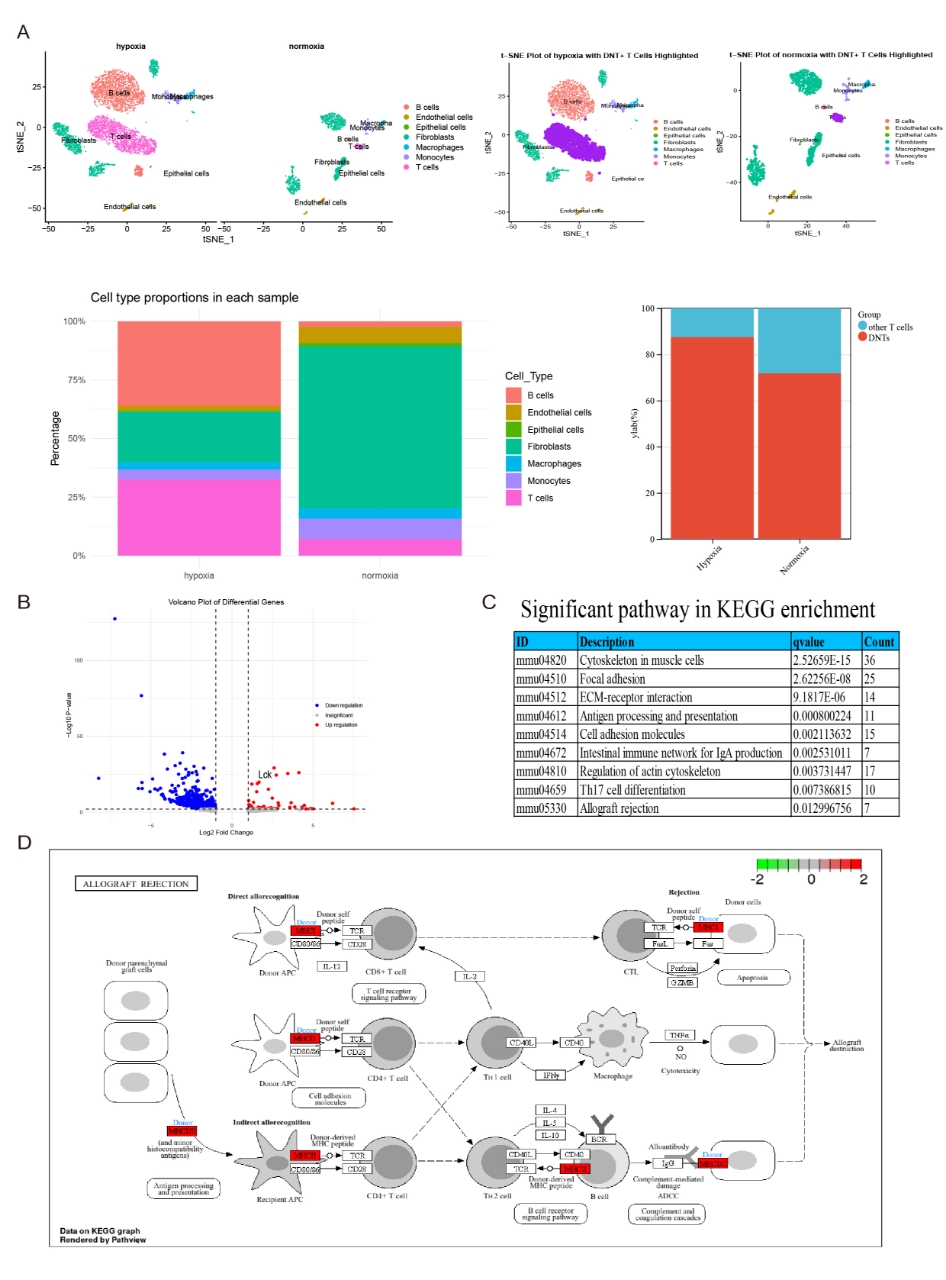
Results: Flow cytometry showed that the proportion of double negative T cells (DNT, CD3+CD56-CD4-CD8-) of patients who died within 28 days after lung transplantation was significantly reduced in peripheral blood (Figure 1.2A), and significantly increased in bronchoalveolar lavage fluid (Figure 1.2B), compared with survivors. The proportion of DNT cells in peripheral blood and lungs showed a significant negative correlation (Figure 1.2C). Transcriptomic validation showed that in chronic lung allograft dysfunction, the DNT specific marker LCK was upregulated (Figure 1.2D), and KEGG analysis showed overactivation of T cells and activation of the graft-versus-host disease pathway in lung allograft dysfunction patients (Figure 1.2D).
Mouse scRNA seq (Figure 2A and 2B) showed hypoxia induced DNT amplification and enhanced expression of activation markers (Lck and Zap70). KEGG pathway analysis identified the overexpression of antigen presentation pathways associated with allogeneic rejection (Figure 2C. 2D. ).
Conclusion: The proportion of DNT cells in peripheral blood and bronchoalveolar lavage fluid is associated with 28 day mortality and lung allograft dysfunction after lung transplantation. Activation of DNT and migration to the lungs in the presence of hypoxia and transplant rejection after lung transplantation. These findings provide novel insights into targeting hypoxia-DNT crosstal improving lung transplant outcomes.
[1] Graft Rejection
[2] lung transplant dysfunction
[3] immune homeostasis
[4] double negative T cell
[5] Allograft Survival