Global survey on system-level barriers that reduce access to transplantation
Andrea Herrera Gayol1, Shaifali Sandal2, Gabriel Gondolesi3, Medhat Askar4, Hari Shankar5, Vivek Kute5, Karen Dwyer6, Kumud Dhital7, Marcelo Cantarovich2.
1AHG Consultant, Westmount, QC, Canada; 2Medicine, McGill University, Montreal, QC, Canada; 3Surgery, Georgetown University , Washington, DC, United States; 4Qatar University, Qatar, Qatar; 5Medicine, Gujarat University, Ahmedabad, India; 6Medicine, Melbourne University, Melbourne , Australia; 7Carditohoracic Surgery, Apollo Hospitals, Bengalore, India
TTS Access to Transplantation working group and the participating transplantation societies.
Introduction: The Global Observatory on Organ Donation and Transplantation (GODT) reported that <10% of the global transplantation (Tx) needs are met.
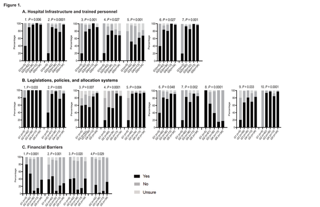
Methods: From May 2022 to March 2023, a survey was conducted, including Tx physicians and surgeons. Responders were grouped as per the mean deceased donation (DD) rate per million population (PMP) from yrs 2016-2021 (excluding 2020 due to the COVID-19 pandemic) into: 1) No DD reported, or no data provided to GODT; 2) <10; 3) 10-19.9; 4) 20-29.9; and 5) ³ 30 DD PMP. Questions about hospital structure, legislative and financial barriers were answered by program directors (PD) as “yes”, “no”, or “unsure”. Fisher exact test was used for statistical analyses.
Results: Significant answers from 150 PD out of 438 responders were the following:
Fig.1.A. Hospital structure 1. Presence of local recovery teams and 2. Local Tx coordinators working in organ donation and Tx (ODT); 3. Strategies to increase the identification of DD, 4. Availability of training programs to manage brain-dead donors, and 5. Donors after circulatory determination of death (DCD); 6. Availability of critical care capacities to manage DD, and 7. Tissue typing laboratories.
Fig.1.B. Legislation, policies, and allocation 1. Regulation of ODT activities, and 2. Brain death confirmation; 3. Policies about end-of-life care; 4. Regulatory mechanisms for donation from DCD and 5. Neurological criteria; 6. Policies on how to approach families and 7. Training counselors; 8. Need to create Tx programs, 9. ODT mandatory registries and 10. Allocation criteria for organ Tx.
Fig 1.C. Financial barriers: 1. Access to Tx, 2. Treatment of post-Tx complications, 3. Adherence to immunosuppression, 4. Gender disparity in the access to Tx.
In general, differences were mainly observed in countries with lower DD rates.
Conclusions: The results of this survey suggest that there are system-level barriers that limit access to Tx. Tackling these challenges may contribute to increasing access to Tx globally.
[1] Hospital structure
[2] Legislation
[3] Financial barriers
[4] Program Directors