Global survey on knowledge and comfort gaps of critical care specialists about deceased donation
Stephen Beed1, Marti Manyalich2, Karen Dwyer3, Hari Shankar4, Marcelo Cantarovich5.
1Medicine, Dalhouise University, Halifax, NS, Canada; 2DTI, Barcelona, Spain; 3Medicine, Melbourne University, Melbourne , Australia; 4Medicine, Gujarat University, Ahmedabad, India; 5Medicine, McGill University, Montreal, QC, Canada
TTS Access to Transplantation working group and the participating transplantation societies.
Introduction: The Global Observatory on Donation and Transplantation (GODT) reported that <10% of the global transplantation (Tx) needs are fulfilled. Critical care physicians play a crucial role in donor identification, diagnosis of neurological death, and donor management. Our goal was to assess their knowledge and comfort gaps about deceased donation (DD).
Methods: A global survey was conducted from May 2022 to March 2023, including critical care specialists. Responders were divided into five groups as per the mean DD rate per million population (PMP) from years 2016-2021 (2020 was excluded because of the COVID-19 pandemic): 1) No DD reported, or no data provided to GODT; 2) <10; 3) 10-19.9; 4) 20-29.9; 5) 30 DD PMP. We used ANOVA (linear trend) to compare the median gap (desired minus current) for knowledge or comfort. As an example: I am aware of the benefits of donation after circulatory determination of death (DCD), but I feel uncomfortable taking care of those donors.
Results: Of 438 responders, 47 (10.7%) included critical care specialists. We found significant differences across countries, in particular in those with lower DD rates. Gaps in knowledge and comfort related to DD included: definition of neurological determination of death (NDD) (Figure 1), and the discussion of donation from NDD with families (Figure 2). Additional significant differences in knowledge and comfort were observed in the following: clinical conditions that may lead to NDD, clinical exam for declaration of NDD, apnea testing for declaration of NDD, indication for ancillary testing in the declaration of NDD, confounders for NDD, evaluation of donor medical suitability and management of DD. Significant differences in knowledge or comfort were seen in the identification and referral of possible DD, in the relative contraindications to DD, and in donation after DCD. No differences were observed in the absolute contraindications to DD.
Conclusion: This survey suggests that there are gaps in knowledge and comfort in various aspects related to DD among critical care specialists. Educational activities should be considered to tackle these gaps to increase DD globally.
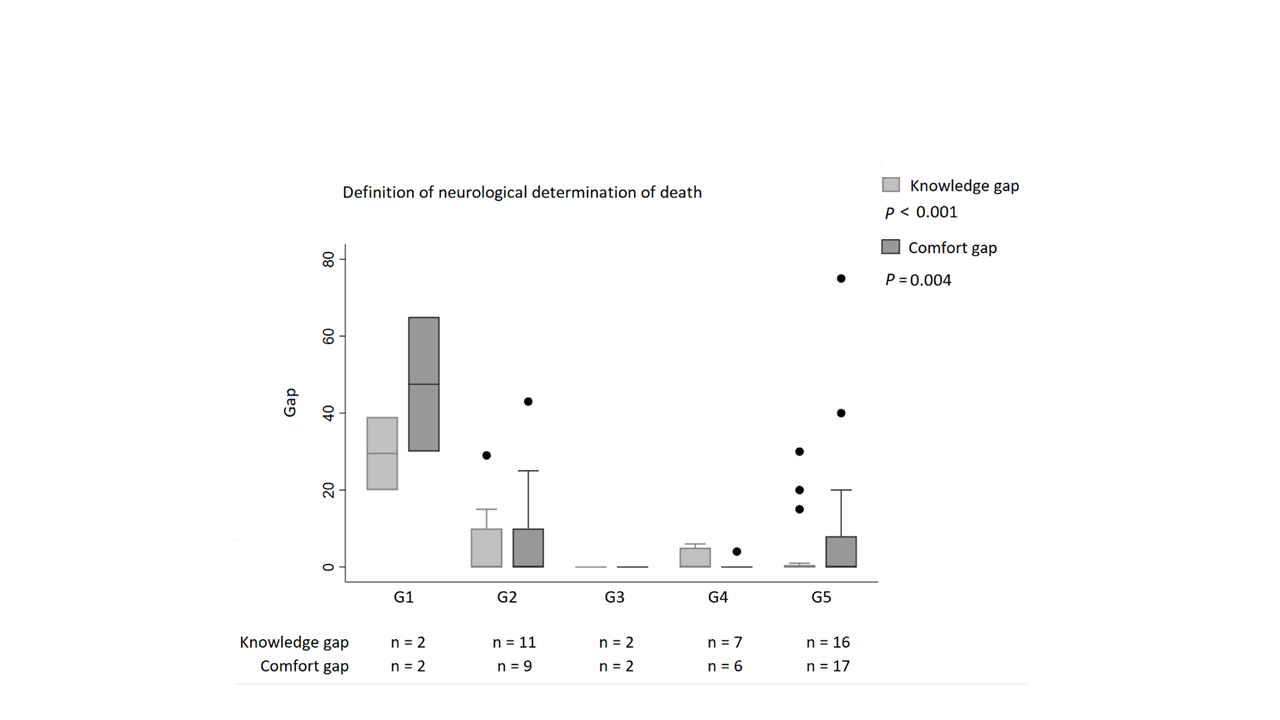
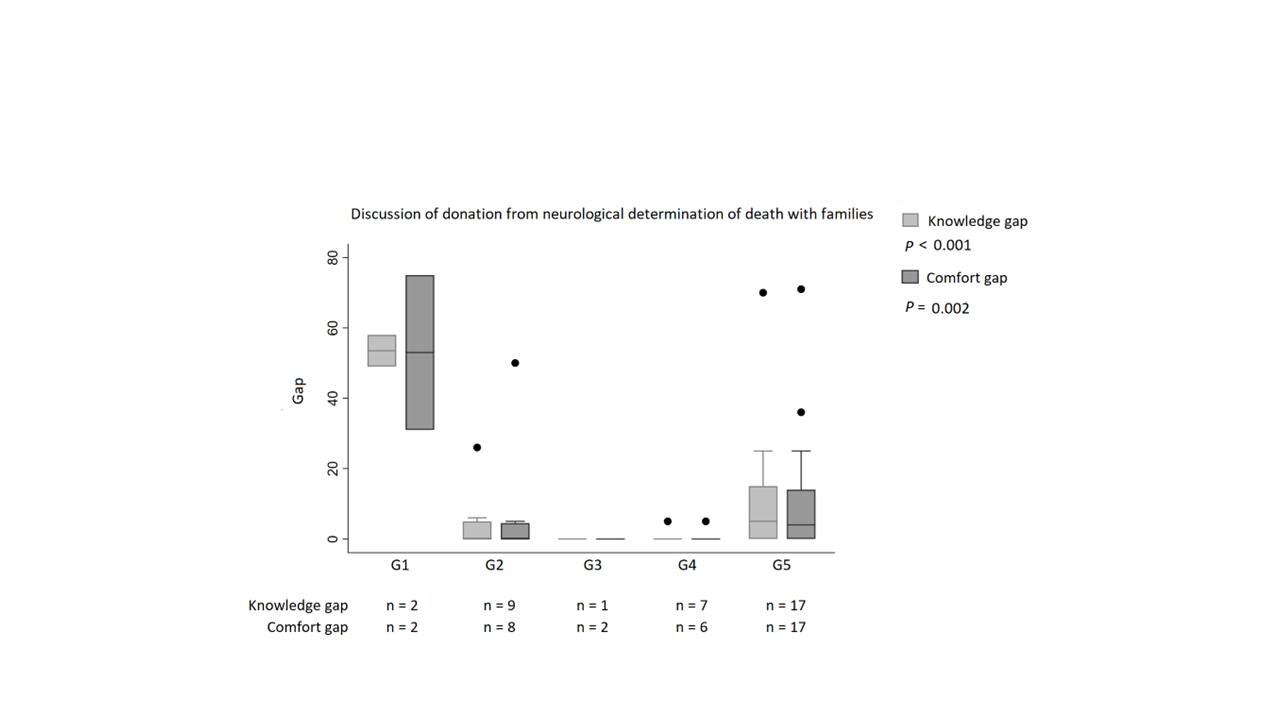
[1] Neurological determination of death
[2] Determination of death by circulatory criteria
[3] Donor identification
[4] Donor management