Ten year exploration of organ donation from the emergency department in the UK
Dale Gardiner1, Sam Richards1, Susanna Madden1, John Richardson1, Olive McGowan1, Dan Harvey1.
1Organ and Tissue Donation and Transplantation, NHS Blood and Transplant, Bristol, United Kingdom
Introduction: Some countries have adopted Intensive Care for Organ Donation (ICOD) which involves admitting patients directly from the Emergency Department, even if non-intubated, specifically to facilitate organ donation. The UK does not permit non-therapeutic (elective) ventilation solely for donation purposes.
In 2018, a UK consensus statement was endorsed by multiple intensive care professional groups, which encouraged the admission of patients with perceived devastating brain injury (DBI) to ICU for neuroprognostication. It recommended that donation only be considered and raised with families after a period of neuroprognostication on ICU.1 This guidance followed cases in which patients initially admitted to ICU for organ donation, following family discussion and agreement in the ED, unexpectedly recovered, with some patients having a good outcome.
We wished to evaluate ten-year donation trends in referral and family approach.
Method: The UK Potential Donor Audit audits deaths in UK Intensive Care Units (ICUs) and Emergency Departments, excluding patients aged over 80 years. Paediatric ICU data are included however neonatal ICU data was excluded. Data were obtained from the national Potential Data Audit (PDA) on all audited deaths in an ED in the UK between 1 April 2015 and 31 March 2025.
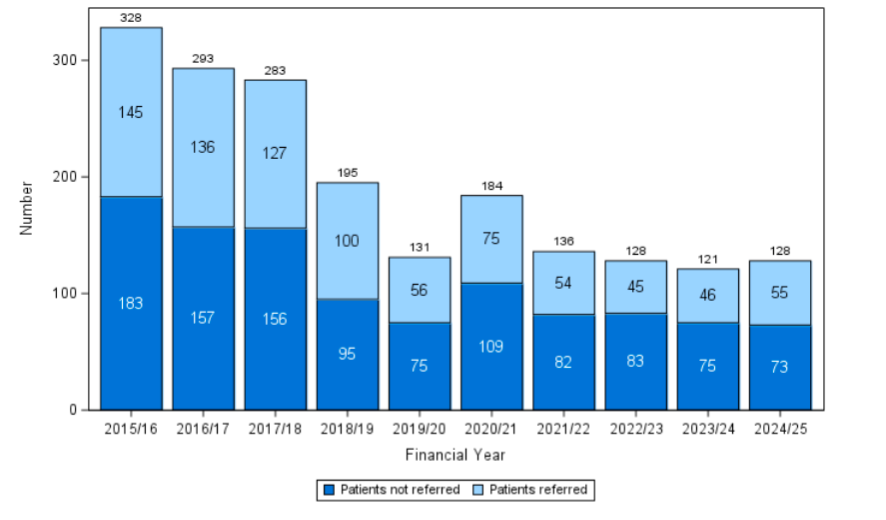
Results: Over the last 10 years, the number of patients who died in the ED meeting referral criteria has decreased, from 328 in 2015/16 to 128 in 2024/25. During the same period the proportion of patients who were not referred has remained similar, 56% in 2015/16 to 57% in 2024/25. In the past year the most common reason for not referring was that the patient was ‘not identified as a potential donor/organ donation not considered’ (n=53, 72.6%).
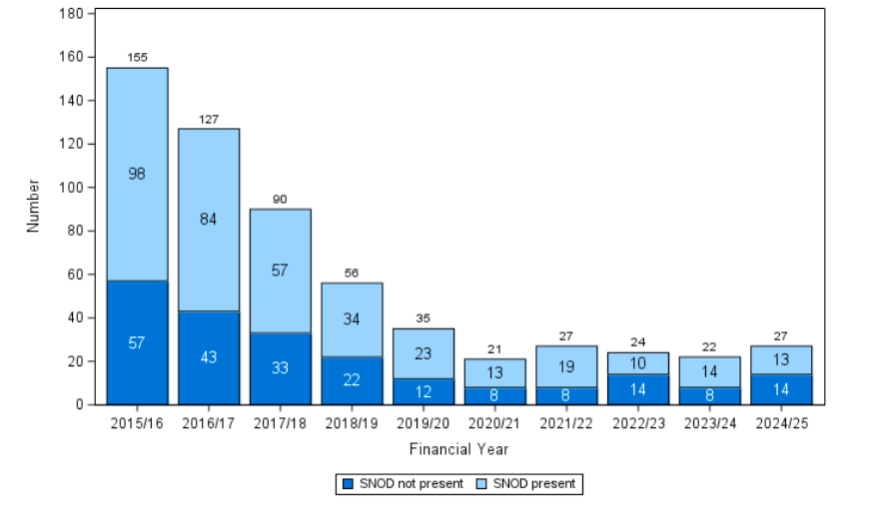
Over the last 10 years, the number of families approached in the ED has decreased, from 155 in 2015/16 to 27 in 2024/25. The proportion of families approached with no Specialist Nurse for Organ Donation (SNOD) present has increased even as the absolute numbers have declined, 37% (n=57) in 2015/16 to 52% (n=14) in 2024/25. In the past year the most common reason for not involving a SNOD in the family approach was ‘planned to proceed without SNOD team member’ (n=5, 35.7%).
Conclusion: There has been a dramatic change in UK practice regarding the care of DBI patients mechanically ventilated in the ED over the last ten years. The number of patients who die meeting referral criteria and the number of families approached for organ donation in ED have both significantly decreased. Instead these patients are being routinely admitted to ICU for neuroprognostication, and if appropriate, consideration for organ donation. Whether the UK would be willing to embrace ICOD for non-intubated patients remains unknown.
References
1. Harvey D, Butler J, Groves J, Manara A, Menon D, Thomas E, Wilson M. Management of perceived devastating brain injury after hospital admission: a consensus statement from stakeholder professional organizations. Br J Anaesth. 2018 Jan;120(1):138-145. doi: 10.1016/j.bja.2017.10.002.
[1] Emergency Department
[2] Donor Identification
[3] Family Approach