Enhancing organ donation outcomes through targeted ICU staff training: evidence from a Dubai based trauma center
Ammar Abdelhadi1,4, Zeyad Alrais1,4, Hanan Obaid4, Maria Gomez2,3, Ali Al Obaidli2, Muneeba Moin1,4, Hisham Abou Alloul2,3, Salome Hernandez1,4, Tawfik Ali1,4.
1Critical care department, Rashid Hospital, Dubai, United Arab Emirates; 2National center for organ donation and transplant, Dubai, United Arab Emirates; 3UAE ministry of health, Dubai, United Arab Emirates; 4Dubai Heath, Dubai, United Arab Emirates
Background: Trauma centers often face unique challenges in organ donation due to the acute nature of cases and the rapid decision making required.
This proposal seeks to explore the impact of specialized training programs for ICU staff, specifically designed to improve donor identification, donor management and family engagement in a culturally diverse setting like Dubai
Objectives: To evaluate the effect of a structured, multi-disciplinary training program for ICU staff on improving outcomes related to organ donation.
The study will assess key metrics, including donor identification rates and family consent rates before and after training.
Methods:
Settings: Conducted between 2021 and 2024 in a high-volume trauma center in Dubai, which handles a significant number of critically injured patients.
Participants: ICU staff including intensivists, nurses and other key personnel involved in in the donor management process.
Intervention: Implementation of a targeted training program focused on four key areas:
Donor identification: to promptly identify clinical criteria of brain death and potential donor suitability.
Donor management: structured protocols for stabilizing and optimizing donors ensuring donor organs viability
Family abroach: communication skills targeted to Dubai’s culturally and religiously unique population to improve family consent rates.
local case studies: to address region specific challenges, such as cultural sensitivity, and legal nuances in organ donation.
Program structure: Delivered through workshops, simulation-based training, and bedside mentoring.
Data collection: Pre and post training comparison of:
Number of potential donors identified and referred to local authorities.
Family consent rates.
Statistical analysis:
Results

Figure 1-1: Referrals Year Over Year (2021–2024)
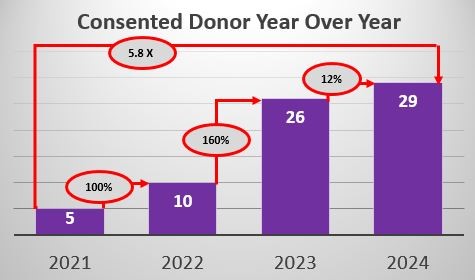
Figure 1-2: Consented Donors Year Over Year (2021–2024)
Interpretation: The referral volume experienced the most significant growth between 2021 and 2022, with gains moderating afterward and stabilizing from 2023 to 2024.
The consented donor count demonstrated exponential growth through 2023, with a decelerated but positive gain in 2024.
Both metrics reflect strong upward trends over the four-year period, suggesting effective staff training impacting referral and donor consent rates.
Discussion: The results demonstrate a significant improvement in organ donation outcomes after implementing the targeted ICU staff training program. The remarkable increase in referral and consented donors suggests that the program was effective in improving donor identification, management, and family engagement.
Conclusion: This study demonstrates the transformative potential of structured ICU staff training on organ donation outcomes in trauma centers, with scalable implications for improving donation rates in diverse and high-pressure clinical environments.