Organ and tissue donation outcomes of an integrated refractory cardiac arrest program including ECMO-CPR (ECPR) and uncontrolled donation after circulatory death (UDCD) in a tertiary university hospital in Spain
Adriana Sánchez Ginés1, Eduard Argudo2, Elisabeth Navas1, Aroa Gómez1, Aurora Gil1, Marianela Guzmán1, Diana Colón1, Maria Vidal3, María Martínez2, Pau Torrella2, Jordi Riera2, Alberto Sandiumenge1.
1Donation and Trasplantation Program Coordination (DTPC), Hospital Universitari Vall d'Hebron, Barcelona, Spain; 2Intensive Care Medicine Department, Hospital Universitari Vall d'Hebron, Barcelona, Spain; 3Cardiology Department, Hospital Universitari Vall d'Hebron, Barcelona, Spain
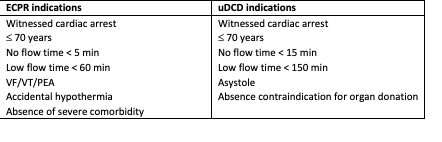
Introduction: A combined ECPR and uncontrolled DCD (uDCD) program has been proposed as a cost-effective strategy to enhance both survival and organ donation outcomes in patients with refractory cardiorespiratory arrest (CRA) 1. In 2023, a pilot initiative integrating these protocols was introduced in three major hospitals in the Barcelona metropolitan area, in collaboration with the regional emergency medical services (SEM). Table 1 summarizes activation criteria. This report details the implementation and clinical activity of one of the participating hospitals.
Methods: Retrospective, observational study including all patients in whom the refractory cardiac arrest protocol -via ECPR or uDCD- was activated between 2022 and 2024 in a large university hospital. The center operates a 24/7 ECPR service and maintains a donor coordination team from 08:00 to 20:00 on weekdays. Patient demographic data, warm-ischemic times (WiT) survival rates, and donation outcomes among non-survivors (brain death-DBD- or controlled (cDCD) and uncontrolled (uDCD) circulatory death) were analysed. Reasons for exclusion from donation, actual donors, and number and types of organs retrieved were also recorded. Results are expressed as mean ± SD or percentages.
Results: A total of 134 activations were recorded :121 ECPR cases (62% out-of-hospital, 38% in-hospital), and 13 uDCD (all out-of-hospital). In the ECPR group, 80% (n=97) were male, mean age 53±14 years. Effective ECMO flow was achieved in 92.5% (n=112), with 29 patients (26%) surviving with good neurological outcome (CPC 1) (WIT: 57,35 ± 24,46 min). Among the 83 non-survivors (WiT: 76,84 ± 24,46 min), 61 (74%) were evaluated for donation; 39 (64%) were considered eligible and 25 were consented for organ and tissue donation (64%). This resulted in 23 organ donors (15 DBD, 8 controlled DCD), yielding 7 lung pairs, 10 livers, 46 kidneys, 18 multi-tissue donors and 50 corneas
Fourteen uDCD cases were activated: 13 at the CRA site, and one at hospital admission post ECPR failure due to prolonged low flow and cannulation dificulties. Most were male (79%; n=11) with a mean age 50±15 years. A total of 10 patients were not converted into actual donors: 3 (25%) didn’t reach the hospital due to logistical issues, 1 case was due to failed cannulation, 3 (25%) presented medical contraindication and 3 (25%) were non consented for donation. Four (29%) patients became effective donors, yielding 8 kidneys (7 utilized), 1 multi-tissue donor and 2 corneas.
Conclusion: The implementation of an integrated program of ECPR and uDCD in our centre enabled survival of 1 out of 4 patients suffering refractory cardiac arrest, and allowed the possibility of donation in 1 out of 5 patients who did not meet the ECPR criteria or who did not survive.