QUALITY score: Development of integrative prognostic index for living donor liver using multicentric registry data
Mun Chae Choi1, Deok-Gie Kim2, Eun-Ki Min2, Jae Geun Lee2, Myoung Soo Kim2, Dong Jin Joo2.
1Surgery, Armed Forces Capital Hospital, Seongnam, Korea; 2Surgery, Yonsei University College of Medicine, Seoul, Korea
Background: Donor factors significantly affect the prognosis of living donor liver transplantation (LDLT). This study aimed to develop integrative prognostic index for living donor liver using Korean Organ Transplantation Registry (KOTRY)
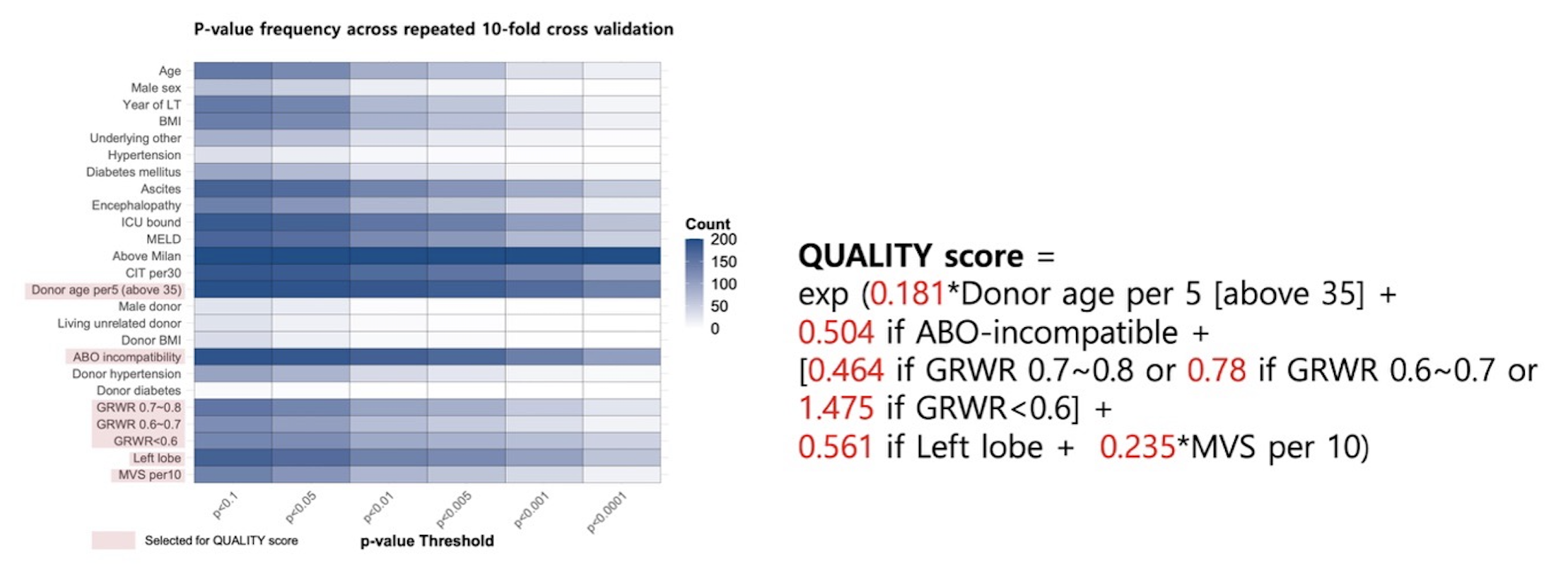
Methods: Data of 4802 eligible LDLT patients was randomly assigned to derivation and validation cohorts with 7:3 ratio. From derivation cohort, six donor variables were selected from 20 times repeated 10-fold cross validation. QUALITY (QUick Assessment of LIving donor liver for LDLT Yeild) score was calculated with mean value of each coefficient adjusted with recipient factors. QUALITY score was then validated the prognostic performance in the validation cohort.
Results: Formula of QUALITY score was “-log10 [exp {(0.167*(Donor age-35)/5) + 0.263 if ABO-incompatible + (0.173 if GRWR 0.7~0.8 or 0.627 if GRWR <0.7) + 0.295 if Other than right lobe + 0.369 if Graft steatosis >=5%)}]*100 +100”.C-indices of QUALITY score were 0.630 in derivation and 0.649 in validation cohort.
Adjusted cubic spline showed linear correlation between QUALITY and graft loss in both cohorts. In the validation cohort, 5-year graft survival was well-stratified by QUALITY score group (90.0% for QUALITY 100 [ideal donor] vs. 87.3% for QUALITY 85-99 vs. 87.1% for QUALITY 70-84 vs. 77.4% for QUALITY 55-69 vs. 68.5% for QUALITY 40-54, P<0.001).
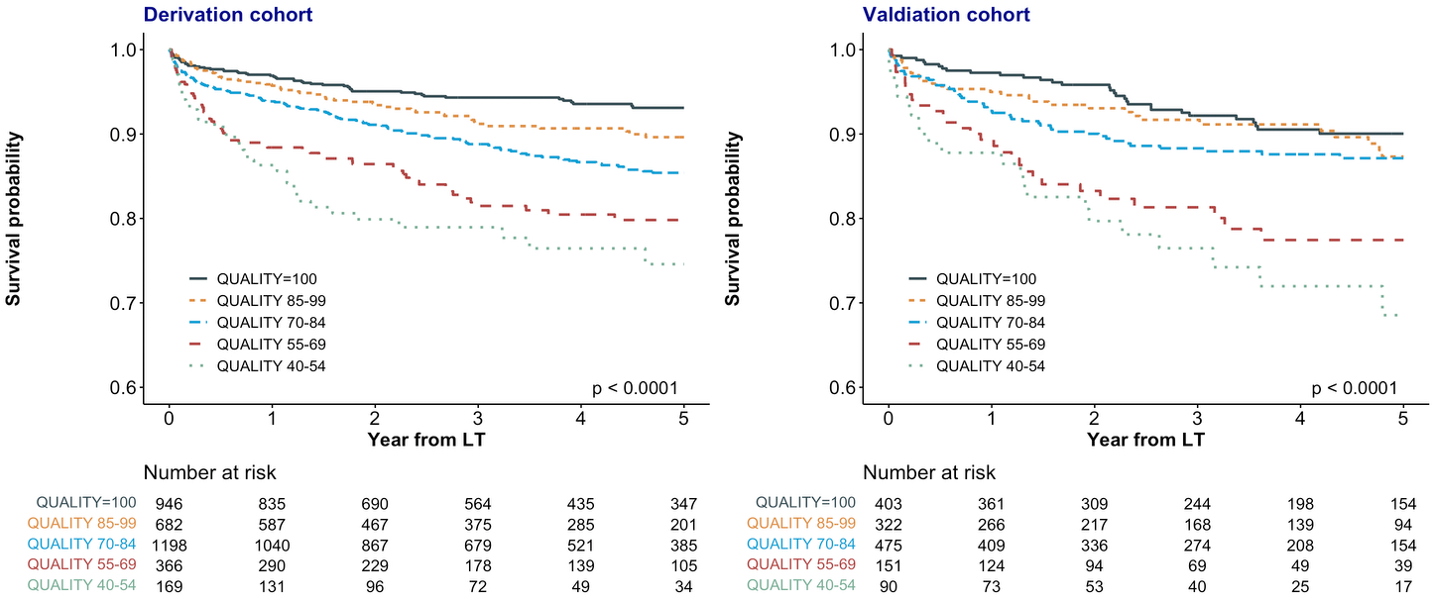
The association of QUALITY and graft survival was independent from recipient risk factors in multivariable analyses (aHR 1.28, 95% CI 1.17-1.39). Predicted graft survival by deciles of QUALITY score was calibrated well with observed survival in the validation cohort. Graft survival after LDLT was more precisely predicted when the QUALITY score was combined with recipient factors such as high MELD, advanced age, ICU bound, and longer cold ischemic time.
Conclusion: QUALITY score provides an intuitive and integrative prognostic assessment of living donor liver independently of the recipient's status. QUALITY score could be used for living donor selection and decision-making regarding whether to proceed with LDLT.
[1] Living donors
[2] Graft survival
[3] Liver transplantation