Data driven quality improvement using grading of donation conversations
Sam Radford1,2, Rohit D'Costa1,3, Matt Ellis1, Shena Graham1.
1DonateLife Victoria, Melbourne, Australia; 2Intensive Care Unit, Austin Health, Melbourne, Australia; 3Intensive Care Unit, Royal Melbourne Hospital, Melbourne, Australia
Introduction: Donor conversations are not created equal. Some are more likely to result in “Yes”. These different conversations require different approaches and evaluation. Stratifying conversations allows for targeted feedback. We describe the development and implementation of a data-driven quality improvement system for Victoria, Australia (population ~6 million, donors per annum 150-190, Registered donor rate ~ 20%).
Method: We developed, evaluated and published a simple prospectively applied model with four grades of conversation, each with different likelihood of consent. Model variables were 1) Registration status on Australian Organ Donor registry (AODR) and 2) donation first raised by staff or family.
Model:
Grade 1: Registered on the AODR, raised by family (least frequent ~ 5%)
Grade 2: Registered on the AODR, raised by staff
Grade 3: Not registered on the AODR, raised by family
Grade 4: Not registered on the AODR, raised by staff (most frequent ~ 70%)
We incorporated our model of grades of consent into our analysis and feedback of referral practices from all hospitals in our jurisdiction.
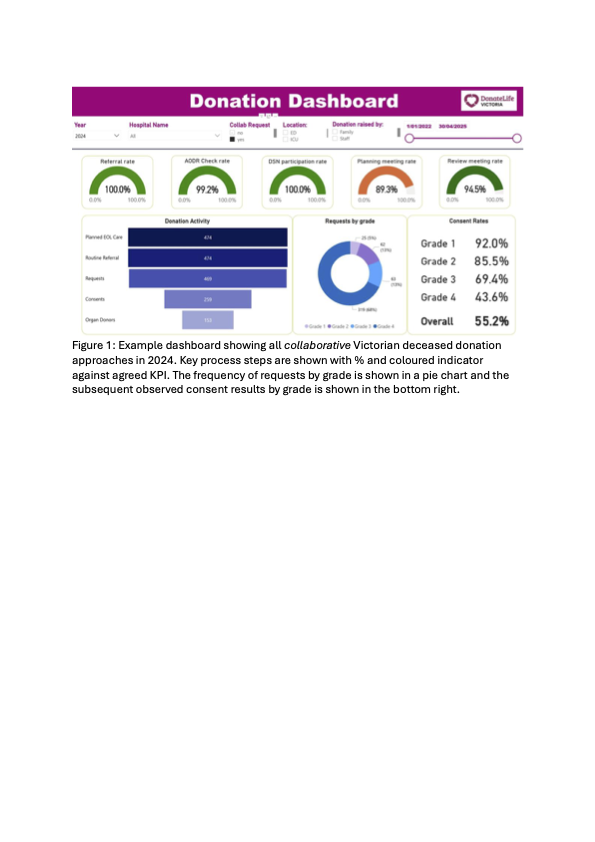
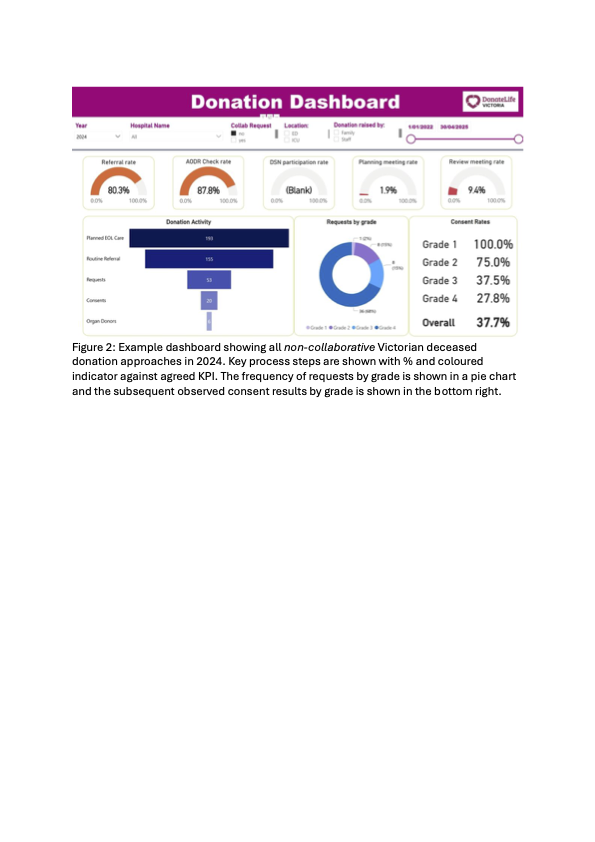
Interactive online dashboards were developed to dynamically review all referring hospitals against agreed best practice standards. Individual case element deviations from best practice were cross checked against the electronic donor record. Constructive feedback and careful enquiry regarding these deviations was provided monthly in a report to relevant clinical and administrative leaders.
We further expanded feedback to include consent rates by grade of conversation. All correspondence now includes the frequency of different grades of conversation plus the observed consent rates with each.
Results: Our initial work demonstrated consent outcomes were significantly different when using collaborative requesting for staff raised conversations (Odds ratio > 2).
The differences in observed consent rates by conversation grade have been sustained before, during and after COVID. Collaborative requesting for staff raised conversations has been embedded as normal practice. In the rare exceptions where non-collaborative conversations occur the observed consent rate is much lower.
Acceptability of results and feedback delivery has been high amongst a variety of stakeholders.
Conclusions: Stratifying conversations into four grades is a practical measure to improve analysis and review of donor family approaches. It allows for comparison of processes and outcomes over time and between locations. It has been associated with the broad acceptance of donation specialist nurses as collaborators in what was previously an Intensive care clinician dominated conversation. Data driven practice improvement has helped develop a shared language and provides a platform for informed review and practice improvement.
[1] Donation Conversation
[2] Collaborative
[3] Donation Specialist
[4] Intensive Care Doctor
[5] Family Approach
[6] Donor Registration
[7] Staff raised
[8] Grades of Conversation
[9] Dashboard
[10] Quality Improvement