Complete referral analysis definitively determines OPO family authorization approach rates by race
J. Thomas Rosenthal1,2, Tom Seto2, Jennifer Prinz3, Jeffrey Trageser4, Sean Van Slyck5, Janice Whaley6, Tom D Mone7.
1Urology, David Geffen School of Medicine at UCLA, Los Angeles, CA, United States; 2OneLegacy, Los Angeles, CA, United States; 3Donor Alliance, Denver, CO, United States; 4Lifesharing, San Diego, CA, United States; 5Sierra Donor Services, Sacramento, CA, United States; 6Donor Network West, San Ramon, CA, United States; 7TDMStrategies, Los Angeles, CA, United States
Introduction: Over the past 5 years OPOs in the United States have been alleged to systematically fail to approach families of color for authorization of organ donation. Two papers published when hospital staff did most of authorization requests have been widely cited as proof. More recent accusations of racial bias came from anonymous statements published in non-peer reviewed editorials, repeated widely in the press, in Congress, and by civil rights organizations. A recent study stated that the odds of being White and approached for authorization were 1.23 times higher than for Blacks and concluded this was evidence of systematic racism in organ donation (AJT. https://doi.org/10.1016/2023.12.024). However, the results were questioned due to concerns with the risk adjustment methodology (AJT; https://doi.org/10.1016/j.ajt.2024.12.012). A method of accurately identifying medically viable potential donors has recently been published, which allows accurate and definitive comparison of family approach rates by race (Transplantation; 2025;109(4):715-719.DOI: 10.1097/TP.0000000000005188).
Methods: Records of all donor referrals made to 5 U.S. OPOs in 2023 were reviewed using the previously described methodology. Referrals were categorized as medical rule-out, missed, or medically acceptable. Medically acceptable referrals approached and not approached were compared by race.
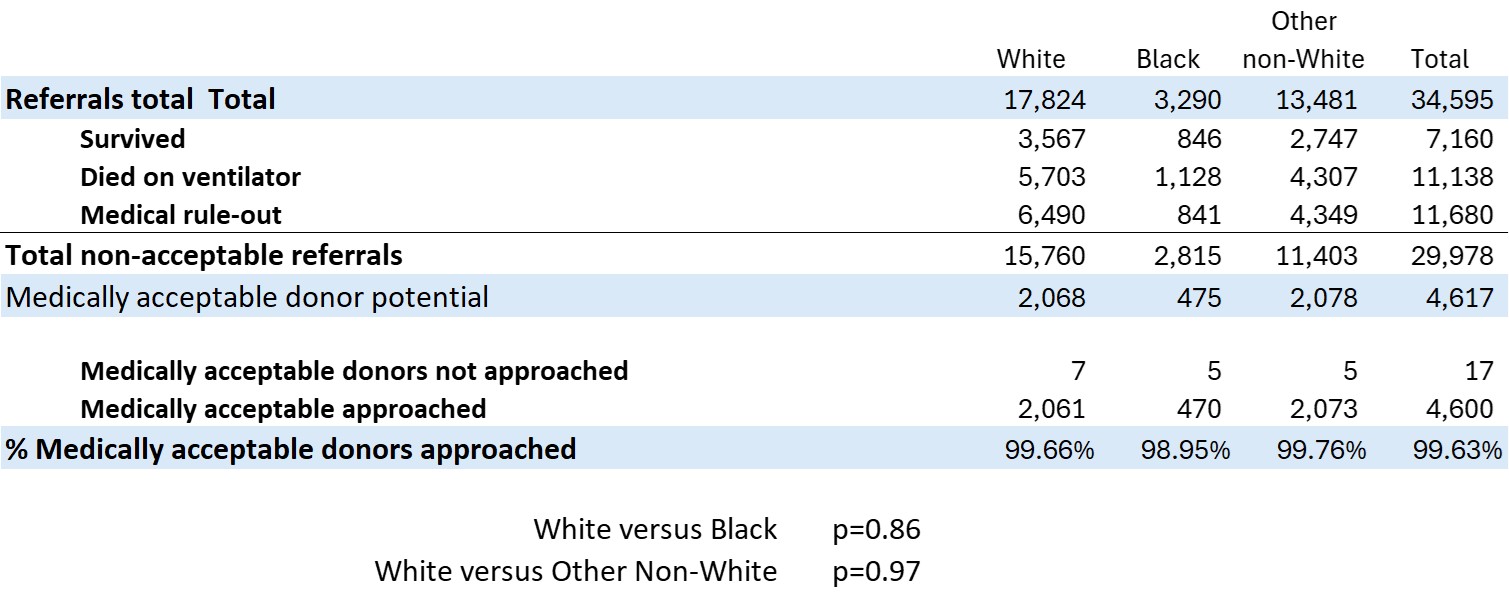
Results: There were 4,617 medically acceptable donors, families of 4,600 were approached for donation authorization and 17 were not approached (0.37% of medically acceptable cases and 0.05% of referrals). Of these, 15 had reflexes present and were expected to survive; 2 did not have clear reasons documented for case closure. There were 7 White, 5 Black, and 5 Other non-White not approached. Overall 99% of medically acceptable potential donors were approached for authorization in each racial group (Table 1). Within each OPO there was no statistical difference between family approaches of White, Black, and other non-White groups.
Approach rates as a percentage of referrals were 11.56% for White, 14.29% for Black, and 15.38% for other non-White. Relative odds ratios from referral to authorization were 0.81 White versus Black and 0.75 White versus Other non-White, both statistically significant (Table 2).
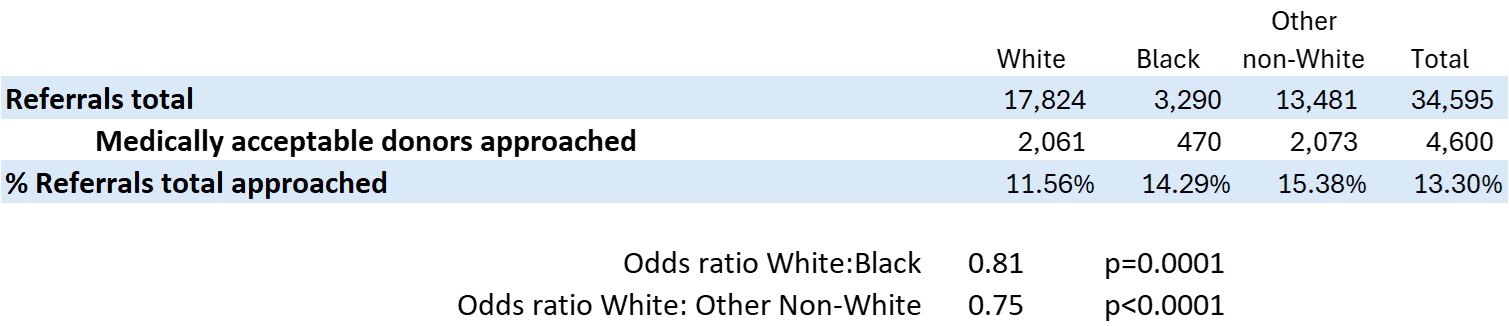
Conclusion: Complete referral analysis is superior to statistical estimation of relative odds of approach. In these five OPOs there was no racial bias in approaching potential donor families for authorization; 99.6% of all medically viable donors were approached with no differences by race. If relative odds of approach were used, there would appear to be a statistically significant different family approach rate for authorization by race, which would be incorrect and misleading. Based on these data, we recommend that complete referral analysis, not statistical risk-adjusted odds ratios, be used to assess OPO approach rates by race.
[1] Referrals
[2] Race