Is India ready for “One India One Allocation Policy” in deceased donor kidney transplant?
Khushboo Saxena1, Subho Banerjee1,2, Anil Kumar3, Vivek Kute1,2, Shiny Suman Pradhan4, Sree Bhushan Raju5,6, Gopalakrishnan Natarajan7,8, Sanjay Kolte2,9,10, Ravi Shetty11, Pranjal Modi12,13, Tukaram Jamale14,15, Gireesh MS16, Ashish Sharma17, Noble Gracious18,19, Vipin Koushal20,21, Kanakeswar Bhuyan22,23, Jigar Shrimali 2,24, Arpita Ray Chaudhury2,25,26, Manish Balwani2,27,28,29.
1Department of Nephrology, Institute of Kidney Disease and Research Centre-Institute of Transplantation Sciences, Ahmedabad, India; 2Executive Council, Indian Society of Organ Transplantation (ISOT), -, India; 3Director, National Organ and Tissue Transplant Organization (NOTTO), Ministry of Health and Family Welfare, Government of India, New Delhi, India; 4National Organ and Tissue Transplant Organization (NOTTO), Ministry of Health and Family Welfare, Government of India, New Delhi, India; 5Department of Nephrology, Nizam's Institute of Medical Sciences, Hyderabad, India; 6Nodal Officer (I/C), Jeevandan Scheme, Telangana, India; 7Member Secretary, Transplant Authority of Tamil Nadu (TRANSTAN), Tamil Nadu, India; 8Director, Regional Organ and Tissue Transplant Organization (ROTTO), -, South, India; 9Director & Head, Department of Urology & Kidney Transplant, Max Hospital, Nagpur, India; 10President, Zonal Transplant Coordination Centre (ZTCC), Nagpur, India; 11Joint Director (Medical), Member Secretary, SOTTO Karnataka, Ministry of Health and Family Welfare, Karnataka, India; 12Department of Urology, Institute of Kidney Disease and Research Centre-Institute of Transplantation Sciences, Ahmedabad, India; 13Convenor, State Organ and Tissue Transplant Organization (SOTTO), Gujarat, India; 14Department of Nephrology, Seth G. S. Medical College and K.E.M. Hospital, Mumbai, India; 15Joint Director In-charge, ROTTO-SOTTO, West, India; 16Department of Nephrology, M.S. Ramaiah Medical College, Bengaluru, India; 17Department of Renal Transplant Surgery, Post Graduate Institute of Medical Education and Research, Chandigarh, India; 18Department of Nephrology, Government Medical College, Thiruvananthapuram, India; 19Executive Director and Member Secretary, SOTTO, Kerala, India; 20Department of Hospital Administration, Post Graduate Institute of Medical Education and Research, Chandigarh, India; 21Nodal Officer, Regional Organ and Tissue Transplant Organization (ROTTO), North, India; 22Professor & Head, Dept of Surgery, Gauhati Medical College & Hospital, Gauhati, India; 23Director , ROTTO Guwahati, Guwahati, India; 24Department of Nephrology, Renus Kidney Hospital, Ahmedabad, India; 25Department of Nephrology, North Bengal Medical College, Siliguri, India; 26President, Indian Society of Organ Transplantation (ISOT), -, India; 27Department of Nephrology, Saraswati Kidney Care Center, Nagpur, India; 28Department of Nephrology, Jawaharlal Nehru Medical College, Sawangi, Wardha, India; 29Secretary , Indian Society of Organ Transplantation (ISOT), -, India
Introduction: Deceased donor kidney transplant (DDKT) program in India an example of the diversity and disparity. Organ donation, utilization and transplants are also disparate between states as are kidney allocation policies. Certain states have pioneering programs with scientifically designed allocation systems. Other programs operate with a “first-come-first-serve” policy. The principles of organ allocation - equality, equity and utility are difficult to balance in settings of low donations. We reviewed the merits of allocation policies across India, the scope of a unifying national policy and propose a way forward.
Methods: We conducted a comprehensive, qualitative comparative analysis of kidney allocation policies across Indian states, using publicly available data and expert input from state and national transplant authorities. Allocation frameworks were assessed based on their incorporation of key ethical principles—equality, equity, and utility—and their practical feasibility within local health ecosystems. Particular focus was placed on point-based systems, medical urgency criteria, sensitization protocols, pediatric and female recipient prioritization, and the recognition of living or deceased donor relatives.
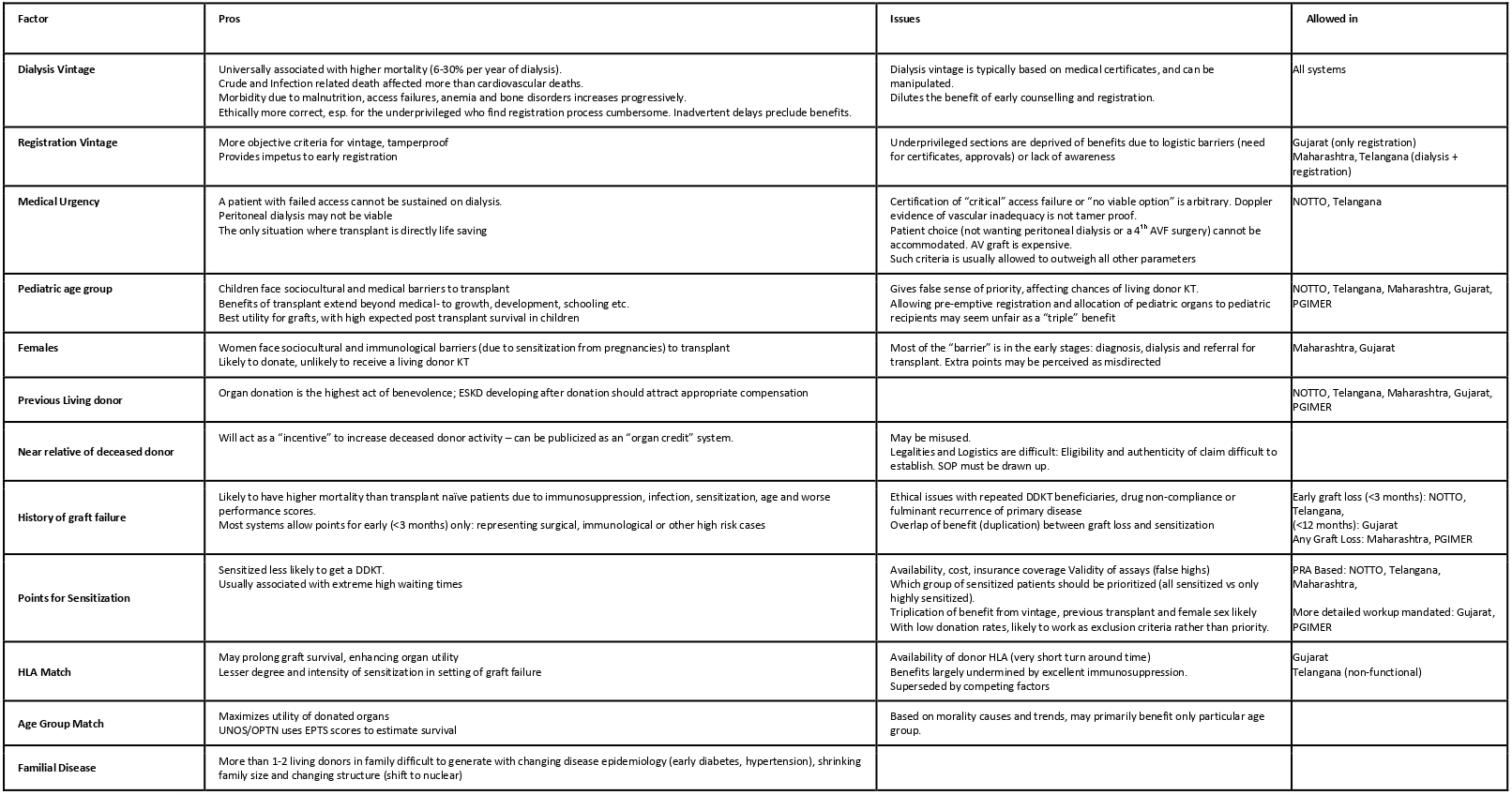
Results: The analysis revealed significant variation in deceased donor kidney allocation policies across Indian states. Most states use dialysis vintage as the primary or sole allocation criterion. In contrast, Gujarat, Maharashtra, and PGIMER Chandigarh have adopted more advanced, multiparameter models incorporating sensitization, pediatric status, female gender, vascular access crisis, and prior donation.
Table 1. Standard parameters used in the deceased donor kidney allocation systems: Pros and Cons
To address this, we propose a tiered recommendation model. For nascent programs, urgent listing for vascular access crisis, seniority-based scoring, and recognition of prior donors and deceased donor families are recommended. Developing programs should additionally prioritize children, females, and patients with early graft failure. Advanced programs should adopt HLA matching, calculated sensitization scoring, acceptable mismatch programs, and list exchanges. This phased approach allows flexibility while aligning with core ethical principles, paving the way for eventual national harmonization.
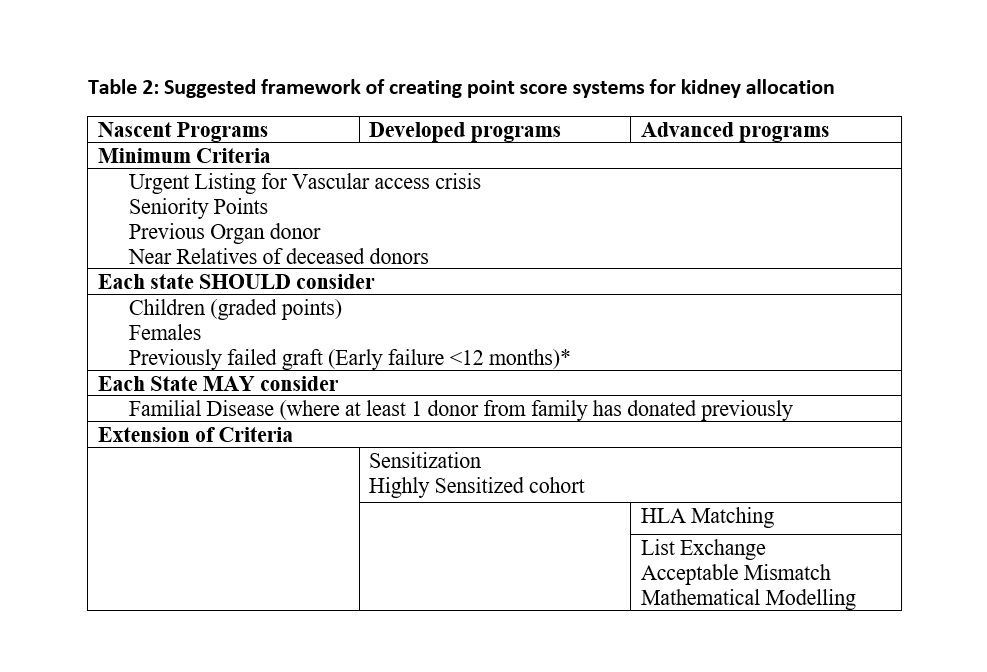
Conclusion: While the basic principles of kidney allocation remain the same, the approach every state needs to take is very different from each other. The aim is to merge into a unifying “One Nation One Allocation” policy. A step-by-step inclusion of various parameters to scientifically allocate kidneys to beneficiaries, and making the process efficient, sustainable and transparent is the only way forward. This Indian experience can be a useful reference for other countries of the South-East Asia region and other developing countries.
[1] allocation policy
[2] deceased donor
[3] kidney transplant
[4] national policy