An ethical approach to anti-obesity interventions in living organ donor candidates
Ali Abbasi1, Alan Zambeli-Ljepovic1, Laura Kimberly2, Peter Stock1, Babak J Orandi3,4.
1Surgery, University of California, San Francisco, San Francisco, CA, United States; 2Department of Population Health, Division of Medical Ethics, New York University Grossman School of Medicine, New York, NY, United States; 3Medicine, New York University Grossman School of Medicine, New York, NY, United States; 4Surgery, New York University Grossman School of Medicine, New York, NY, United States
Introduction: The number of living organ donors in the US and Europe has stagnated for 20 years, in part due to the rising prevalence of obesity, a common disqualifying comorbidity. While anti-obesity medications and surgery could help potential donors lose weight prior to donation, these interventions create a number of ethical concerns. Weight regain is common when stopping anti-obesity medications, which could expose potential donors to significant health risks after nephrectomy. In addition, in many countries access to anti-obesity medicines is limited by payment policies. Therefore, giving preferential access to living donors could be coercive. Here, we propose an ethical approach to implementation of anti-obesity interventions in living donor candidates.
Methods: In a multi-disciplinary collaboration involving transplant professionals, obesity medicine experts, and medical ethicists, we conducted a normative analysis of ethical and policy implications of anti-obesity therapy for prospective living donors, grounded in the fundamental principles of medical ethics: beneficence, non-maleficence, autonomy, and justice. Based on these principles, we derive ethical and policy recommendations for the ethical implementation of anti-obesity therapy as part of living donor care.
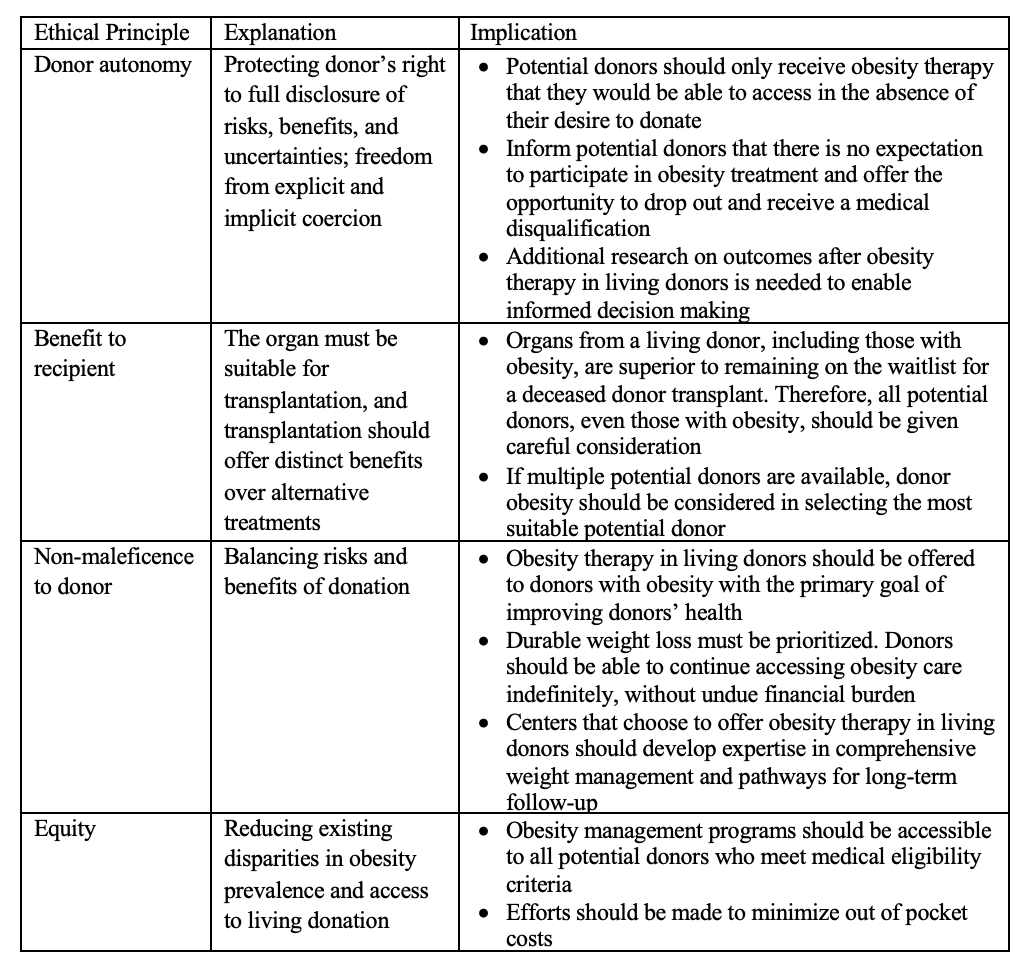
Results: The fundamental principles of medical ethics require transplant professionals to maximize benefits to the recipient, protect donor autonomy, balance the risks and benefits to the donor, and promote fair access to transplantation (Figure 1). When applied to anti-obesity interventions in living donors, maximizing benefits to the recipient calls for evaluating all potential living donors, including those with obesity. Balancing risks and benefits to the donor requires transplant professionals to focus on strategies that can result in durable weight loss and sustainable access to weight loss therapies. Donor autonomy can be protected by ensuring potential donors only receive therapies that they would be eligible for in the absence of the desire to donate. Promoting equity calls for focusing on weight loss strategies that are eligible to all patients, regardless of financial resources. Based on these considerations, we identify policy recommendations for transplant organizations, transplant centers, and government bodies. Consensus recommendations by transplant organizations could be helpful facilitate ethical implementation of anti-obesity interventions in living donors.
Conclusions: Anti-obesity therapies may increase the number of living donations and improve equity in transplantation, but guidance is needed to balance the ethical tensions between the obesity medicine landscape, payment policies, and the transplant system.